Внутрь, после еды, по 0,2 мг 3 раза в сутки в течение 2 дней или по 0,2–0,3 мг в сутки в течение 4 дней; при поддерживающей терапии — по 0,2–0,3 мг/сут (по возможности утром). Для быстрого насыщения Lanoxinом — в/в 2–4 ампулы (0,2 мг/мл) в средней суточной дозе 0,6 мг в течение 3-х дней, далее пациентов переводят на прием таблеток.
Редко: потеря аппетита, диспептические расстройства, инфаркт брыжейки, аритмии (в т.ч. желудочковая тахикардия, экстрасистолия, AV блокада I-III степени), головные боли, нарушения сна, зрения, дезориентация, депрессия, психозы, афазия, мышечные боли, аллергические реакции.
Инъецируемый; Раствор для инъекций; Раствор; Раствор для инфузий
Хроническая сердечная недостаточность; мерцательная тахиаритмия, пароксизмальная наджелудочковая тахикардия.
Гиперчувствительность, интоксикация дигиталисом, гипертрофическая обструктивная кардиомиопатия, желудочковая тахикардия, AV-блокада II и III степени (без водителя ритма), WPW-синдром, гиперкальциемия, гипокалиемия, аневризма грудного отдела аорты, синдром каротидного синуса.
Не рекомендуется (особенно в I триместре беременности).
Увеличивает силу и скорость сердечных сокращений, урежает их частоту, замедляет AV проводимость.
- Сердечные гликозиды и негликозидные кардиотонические средства
Эффект могут усиливать кальций, пенициллины, амфотерицин B, тетрациклины, макролиды, карбеноксолон, глюкокортикоиды, АКТГ, салицилаты, антиаритмики (хинидин, амиодарон, бета-адреноблокаторы и др.), каптоприл, резерпин, тиреостатические препараты, ослаблять — антагонисты кальция, соли калия, калийсберегающие диуретики, препараты, снижающие резорбцию из ЖКТ (активированный уголь, холестирамин, колестипол, антациды, каолин-пептиды), неомицин, парааминосалициловая кислота, цитостатики, сульфасалазин, фенитоин, метоклопрамид, НПВС, тиреоидные гормоны. Одновременное применение с симпатомиметиками, циклопропаном, резерпином, трициклическими антидепрессантами, ингибиторами фосфодиэстеразы, суксаметонием хлоридом повышает вероятность развития аритмии.
При температуре не выше 30 °C.
Хранить в недоступном для детей месте.
Срок годности препарата Дигоксин3 года.
Не применять по истечении срока годности, указанного на упаковке.
Инструкция по медицинскому применению Дигоксин — инструкция по медицинскому применению — РУ № ЛП-000051 от 2015-11-25
Дигоксин — инструкция по медицинскому применению — РУ № ЛП-000051 от 2010-11-24
| Таблетки | 1 табл. |
| дигоксин | 0,25 мг |
| вспомогательные вещества: кремнезем коллоидный безводный; магния стеарат; желатин; тальк; крахмал кукурузный; лактозы моногидрат |
во флаконах по 50 шт.; в коробке 1 флакон.
Оставьте отзыв
Оставлять отзывы могут только авторизованные пользователи. Пожалуйста, авторизуйтесь
Способ применения и дозировка
Внутрь. При среднебыстрой дигитализации: в 1 день — 1,5 мг, во 2 — 0,9 мг, с 3 по 5 — по 0,75 мг. При медленной дигитализации в первые 4 дня — по 0,75 мг, с 5 по 7 день — по 0,5 мг. Поддерживающая доза — 0,25-0,5 мг в сутки. Детям до 14 лет — 0,025-0,075 мг на кг.
Условия хранения
Хранить при комнатной температуре в сухом, защищенном от света и недоступном для детей месте.
Состав
Активное вещество — дигоксин.
Передозировка
Симптомы: Аритмия, AV блокада, рвота, тошнота.
Лечение: препараты калия, унитиол, этилендиаминтетраацетат.
Особые указания
С осторожностью комбинируют с диуретиками, симпатомиметиками. Следует избегать совместного назначения с амфотерицином В и препаратами кальция.
Взаимодействие
Адреномиметики увеличивают вероятность развития аритмии, антиаритмические и антихолинэстеразные препараты — брадикардии, глюкокортикоиды, салуретики и др. средства, способствующие потере калия, препараты кальция — гликозидной интоксикации. Аминазин уменьшает кардиотонический эффект, слабительные, антациды, средства, содержащие алюминий, висмут, магний, — всасывание. Рифампицин и сульфасалазин ускоряют метаболизм.
Фармакологическое действие
Кардиостимулирующее, антиаритмическое. Оказывает положительное инотропное, отрицательное хроно- и дромотропное, положительное батмотропное (в токсических дозах). Хорошо всасывается при приеме внутрь. Равномерно распределяется по органам и тканям. Часть выделяется в двенадцатиперстную кишку с желчью и подвергается реабсорбции. Способен кумулировать. Связывается с белками плазмы на 35-40%. Экскретируется преимущественно с мочой (при беременности — замедленно). У больных с хронической сердечной недостаточностью вызывает опосредованную вазодилатацию, умеренно повышает диурез (в основном за счет улучшения гемодинамики). После приема внутрь кардиотонический эффект развивается через 1-2 часа, достигает максимума в течение 8 часов, после внутривенного введения — через 20-30 мин. У больных с ненарушенными функциями печени и почек действие прекращается через 2-7 дней.
Показания к применению
Застойная недостаточность кровообращения (без гемодинамически значимой обструкции выходного тракта сердца), мерцательная тахиаритмия, суправентрикулярная пароксизмальная тахикардия, трепетание предсердий.
Побочное действие
Тошнота, рвота, анорексия, брадикардия, желудочковая экстрасистолия, AV блокада, головная боль, головокружение. Возможно нарушение цветового зрения, снижение остроты зрения, скотомы, макро- и микроопсия, при длительном применении — гинекомастия.
Противопоказания
Гликозидная интоксикация.
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use LANOXIN safely and effectively. See full prescribing information for LANOXIN.
LANOXIN® (digoxin) tablets, for oral use
Initial U.S. Approval: 1954
INDICATIONS AND USAGE
LANOXIN is a cardiac glycoside indicated for:
- Treatment of mild to moderate heart failure in adults. (1.1)
- Increasing myocardial contractility in pediatric patients with heart failure. (1.2)
- Control of resting ventricular rate in patients with chronic atrial fibrillation in adults. (1.3)
DOSAGE AND ADMINISTRATION
LANOXIN dose is based on patient-specific factors (age, lean body weight, renal function, etc.). See full prescribing information. Monitor for toxicity and therapeutic effect. (2)
DOSAGE FORMS AND STRENGTHS
Unscored Tablets: 62.5 mcg. Scored Tablets 125 and 250 mcg. (3)
CONTRAINDICATIONS
- Ventricular fibrillation. (4)
- Known hypersensitivity to digoxin or other forms of digitalis. (4)
WARNINGS AND PRECAUTIONS
- Risk of rapid ventricular response leading to ventricular fibrillation in patients with AV accessory pathway. (5.1)
- Risk of advanced or complete heart block in patients with sinus node disease and AV block. (5.2)
- Digoxin toxicity: Indicated by nausea, vomiting, visual disturbances, and cardiac arrhythmias. Advanced age, low body weight, impaired renal function and electrolyte abnormalities predispose to toxicity. (5.3)
- Risk of ventricular arrhythmias during electrical cardioversion. (5.4)
- Not recommended in patients with acute myocardial infarction. (5.5)
- Avoid LANOXIN in patients with myocarditis. (5.6)
ADVERSE REACTIONS
The overall incidence of adverse reactions with digoxin has been reported as 5-20%, with 15-20% of adverse events considered serious. Cardiac toxicity accounts for about one-half, gastrointestinal disturbances for about one-fourth, and CNS and other toxicity for about one-fourth of these adverse events. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Advanz Pharma (US) Corp. at 1-877-370-1142 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
DRUG INTERACTIONS
- PGP Inducers/Inhibitors: Drugs that induce or inhibit PGP have the potential to alter digoxin pharmacokinetics. (7.1)
- The potential for drug-drug interactions must be considered prior to and during drug therapy. See full prescribing information. (7.2, 7.3, 12.3)
USE IN SPECIFIC POPULATIONS
- Pregnant patients: It is unknown whether use during pregnancy can cause fetal harm. (8.1)
- Pediatric patients: Newborn infants display variability in tolerance to LANOXIN. (8.4)
- Geriatric patients: Consider renal function in dosage selection, and carefully monitor for side effects. (8.5)
- Renal impairment: LANOXIN is excreted by the kidneys. Consider renal function during dosage selection. (8.6)
See 17 for PATIENT COUNSELING INFORMATION.
Revised: 12/2024
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1 INDICATIONS AND USAGE
1.1 Heart Failure in Adults
1.2 Heart Failure in Pediatric Patients
1.3 Atrial Fibrillation in Adults
2 DOSAGE AND ADMINISTRATION
2.1 Important Dosing and Administration Information
2.2 Loading Dosing Regimen in Adults and Pediatric Patients
2.3 Maintenance Dosing in Adults and Pediatric Patients Over 10 Years Old
2.4 Maintenance Dosing in Pediatric Patients Less Than 10 Years Old
2.5 Monitoring to Assess Safety, Efficacy, and Therapeutic Blood Levels
2.6 Switching from Intravenous Digoxin to Oral Digoxin
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Ventricular Fibrillation in Patients With Accessory AV Pathway (Wolff-Parkinson-White Syndrome)
5.2 Sinus Bradycardia and Sino-atrial Block
5.3 Digoxin Toxicity
5.4 Risk of Ventricular Arrhythmias During Electrical Cardioversion
5.5 Risk of Ischemia in Patients With Acute Myocardial Infarction
5.6 Vasoconstriction In Patients With Myocarditis
5.7 Decreased Cardiac Output in Patients With Preserved Left Ventricular Systolic Function
5.8 Reduced Efficacy In Patients With Hypocalcemia
5.9 Altered Response in Thyroid Disorders and Hypermetabolic States
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
7 DRUG INTERACTIONS
7.1 P-Glycoprotein (PGP) Inducers/Inhibitors
7.2 Pharmacokinetic Drug Interactions
7.3 Potentially Significant Pharmacodynamic Drug Interactions
7.4 Drug/Laboratory Test Interactions
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Renal Impairment
8.7 Hepatic Impairment
8.8 Malabsorption
10 OVERDOSAGE
10.1 Signs and Symptoms in Adults and Children
10.2 Treatment
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
14.1 Chronic Heart Failure
14.2 Chronic Atrial Fibrillation
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
- *
- Sections or subsections omitted from the full prescribing information are not listed.
-
1 INDICATIONS AND USAGE
1.1 Heart Failure in Adults
LANOXIN is indicated for the treatment of mild to moderate heart failure in adults. LANOXIN increases left ventricular ejection fraction and improves heart failure symptoms as evidenced by improved exercise capacity and decreased heart failure-related hospitalizations and emergency care, while having no effect on mortality. Where possible, LANOXIN should be used in combination with a diuretic and an angiotensin-converting enzyme (ACE) inhibitor.
1.2 Heart Failure in Pediatric Patients
LANOXIN increases myocardial contractility in pediatric patients with heart failure.
1.3 Atrial Fibrillation in Adults
LANOXIN is indicated for the control of ventricular response rate in adult patients with chronic atrial fibrillation.
-
2 DOSAGE AND ADMINISTRATION
2.1 Important Dosing and Administration Information
In selecting a LANOXIN dosing regimen, it is important to consider factors that affect digoxin blood levels (e.g., body weight, age, renal function, concomitant drugs) since toxic levels of digoxin are only slightly higher than therapeutic levels. Dosing can be either initiated with a loading dose followed by maintenance dosing if rapid titration is desired or initiated with maintenance dosing without a loading dose.
Consider interruption or reduction in LANOXIN dose prior to electrical cardioversion [see Warnings and Precautions (5.4)].
Use digoxin solution to obtain the appropriate dose in infants, young pediatric patients, or patients with very low body weight.
2.2 Loading Dosing Regimen in Adults and Pediatric Patients
For adults and pediatric patients if a loading dosage is to be given, administer half the total loading dose initially, then ¼ the loading dose every 6-8 hours twice, with careful assessment of clinical response and toxicity before each dose. The recommended loading dose is displayed in Table 1.
mcg = microgram
2.3 Maintenance Dosing in Adults and Pediatric Patients Over 10 Years Old
The maintenance dose is based on lean body weight, renal function, age, and concomitant products [see Clinical Pharmacology (12.3)].
The recommended starting maintenance dose in adults and pediatric patients over 10 years old with normal renal function is given in Table 2. Doses may be increased every 2 weeks according to clinical response, serum drug levels, and toxicity.
mcg = microgram
Table 3 provides the recommended (once daily) maintenance dose for adults and pediatric patients over 10 years old (to be given once daily) according to lean body weight and renal function. The doses are based on studies in adult patients with heart failure. Alternatively, the maintenance dose may be estimated by the following formula (peak body stores lost each day through elimination):
Total Maintenance Dose = Loading Dose (i.e., Peak Body Stores) x % Daily Loss/100
(% Daily Loss = 14 + Creatinine clearance/5)Reduce the dose of LANOXIN in patients whose lean weight is an abnormally small fraction of their total body mass because of obesity or edema.
a Doses are rounded to the nearest dose possible using whole LANOXIN tablets. Recommended doses approximately 30 percent lower than the calculated dose are designated with an *. Monitor digoxin levels in patients receiving these initial doses and increase dose if needed.
bFor adults, creatinine clearance was corrected to 70-kg body weight or 1.73 m2 body surface area. If only serum creatinine concentrations (Scr) are available, a corrected Ccr may be estimated in men as (140 – Age)/Scr. For women, this result should be multiplied by 0.85.
For pediatric patients, the modified Schwartz equation may be used. The formula is based on height in cm and Scr in mg/dL where k is a constant. Ccr is corrected to 1.73 m2 body surface area. During the first year of life, the value of k is 0.33 for pre-term babies and 0.45 for term infants. The k is 0.55 for pediatric patients and adolescent girls and 0.7 for adolescent boys.
GFR (mL/min/1.73 m2) = (k x Height)/Scr
c If no loading dose administered.
d The doses listed assume average body composition.2.4 Maintenance Dosing in Pediatric Patients Less Than 10 Years Old
The starting maintenance dose for heart failure in pediatric patients less than 10 years old is based on lean body weight, renal function, age, and concomitant products [see Clinical Pharmacology (12.3)]. The recommended starting maintenance dose for pediatric patients between 5 years and 10 years old is given in Table 4. These recommendations assume the presence of normal renal function.
Table 5 provides average daily maintenance dose requirements for pediatric patients between 5 and 10 years old (to be given twice daily) with heart failure based on age, lean body weight, and renal function.
a Recommended are doses to be given twice daily.
b The doses are rounded to the nearest dose possible using whole LANOXIN tablets. Recommended doses approximately 30 percent lower than the calculated dose are designated with an *. Monitor digoxin levels in patients receiving these initial doses and increase dose if needed.
c The modified Schwartz equation may be used to estimate creatinine clearance. See footnote b under Table 3.
d If no loading dose administered.2.5 Monitoring to Assess Safety, Efficacy, and Therapeutic Blood Levels
Monitor for signs and symptoms of digoxin toxicity and clinical response. Adjust dose based on toxicity, efficacy, and blood levels.
Serum digoxin levels less than 0.5 ng/mL have been associated with diminished efficacy, while levels above 2 ng/mL have been associated with increased toxicity without increased benefit.
Interpret the serum digoxin concentration in the overall clinical context, and do not use an isolated measurement of serum digoxin concentration as the basis for increasing or decreasing the LANOXIN dose. Serum digoxin concentrations may be falsely elevated by endogenous digoxin-like substances [see Drug Interactions (7.4)]. If the assay is sensitive to these substances, consider obtaining a baseline digoxin level before starting LANOXIN and correct post-treatment values by the reported baseline level.
Obtain serum digoxin concentrations just before the next scheduled LANOXIN dose or at least 6 hours after the last dose. The digoxin concentration is likely to be 10-25% lower when sampled right before the next dose (24 hours after dosing) compared to sampling 8 hours after dosing (using once-daily dosing). However, there will be only minor differences in digoxin concentrations using twice daily dosing whether sampling is done at 8 or 12 hours after a dose.
2.6 Switching from Intravenous Digoxin to Oral Digoxin
When switching from intravenous to oral digoxin formulations, make allowances for differences in bioavailability when calculating maintenance dosages (see Table 6).
-
3 DOSAGE FORMS AND STRENGTHS
Unscored Tablets: 62.5 mcg are peach, round with «U3A» imprinted on one side.
Scored Tablets: 125 mcg are yellow, round, scored tablets with «Y3B» imprinted on one side.
Scored Tablets: 250 mcg are white, round, scored tablets with «X3A» imprinted on one side. -
4 CONTRAINDICATIONS
LANOXIN is contraindicated in patients with:
- Ventricular fibrillation [see Warnings and Precautions (5.1)]
- Known hypersensitivity to digoxin (reactions seen include unexplained rash, swelling of the mouth, lips or throat or a difficulty in breathing). A hypersensitivity reaction to other digitalis preparations usually constitutes a contraindication to digoxin.
-
5 WARNINGS AND PRECAUTIONS
5.1 Ventricular Fibrillation in Patients With Accessory AV Pathway (Wolff-Parkinson-White Syndrome)
Patients with Wolff-Parkinson-White syndrome who develop atrial fibrillation are at high risk of ventricular fibrillation. Treatment of these patients with digoxin leads to greater slowing of conduction in the atrioventricular node than in accessory pathways, and the risks of rapid ventricular response leading to ventricular fibrillation are thereby increased.
5.2 Sinus Bradycardia and Sino-atrial Block
LANOXIN may cause severe sinus bradycardia or sinoatrial block particularly in patients with pre-existing sinus node disease and may cause advanced or complete heart block in patients with pre-existing incomplete AV block. Consider insertion of a pacemaker before treatment with digoxin.
5.3 Digoxin Toxicity
Signs and symptoms of digoxin toxicity include anorexia, nausea, vomiting, visual changes and cardiac arrhythmias [first-degree, second-degree (Wenckebach), or third-degree heart block (including asystole); atrial tachycardia with block; AV dissociation; accelerated junctional (nodal) rhythm; unifocal or multiform ventricular premature contractions (especially bigeminy or trigeminy); ventricular tachycardia; and ventricular fibrillation]. Toxicity is usually associated with digoxin levels greater than 2 ng/ml although symptoms may also occur at lower levels. Low body weight, advanced age or impaired renal function, hypokalemia, hypercalcemia, or hypomagnesemia may predispose to digoxin toxicity. Obtain serum digoxin levels in patients with signs or symptoms of digoxin therapy and interrupt or adjust dose if necessary [see Adverse Reactions (6) and Overdosage (10)]. Assess serum electrolytes and renal function periodically.
The earliest and most frequent manifestation of digoxin toxicity in infants and children is the appearance of cardiac arrhythmias, including sinus bradycardia. In children, the use of digoxin may produce any arrhythmia. The most common are conduction disturbances or supraventricular tachyarrhythmias, such as atrial tachycardia (with or without block) and junctional (nodal) tachycardia. Ventricular arrhythmias are less common. Sinus bradycardia may be a sign of impending digoxin intoxication, especially in infants, even in the absence of first-degree heart block. Any arrhythmias or alteration in cardiac conduction that develops in a child taking digoxin should initially be assumed to be a consequence of digoxin intoxication.
Given that adult patients with heart failure have some symptoms in common with digoxin toxicity, it may be difficult to distinguish digoxin toxicity from heart failure. Misidentification of their etiology might lead the clinician to continue or increase LANOXIN dosing, when dosing should actually be suspended. When the etiology of these signs and symptoms is not clear, measure serum digoxin levels.
5.4 Risk of Ventricular Arrhythmias During Electrical Cardioversion
It may be desirable to reduce the dose of or discontinue LANOXIN for 1 to 2 days prior to electrical cardioversion of atrial fibrillation to avoid the induction of ventricular arrhythmias, but physicians must consider the consequences of increasing the ventricular response if digoxin is decreased or withdrawn. If digitalis toxicity is suspected, elective cardioversion should be delayed. If it is not prudent to delay cardioversion, the lowest possible energy level should be selected to avoid provoking ventricular arrhythmias.
5.5 Risk of Ischemia in Patients With Acute Myocardial Infarction
LANOXIN is not recommended in patients with acute myocardial infarction because digoxin may increase myocardial oxygen demand and lead to ischemia.
5.6 Vasoconstriction In Patients With Myocarditis
LANOXIN can precipitate vasoconstriction and may promote production of pro-inflammatory cytokines; therefore, avoid use in patients with myocarditis.
5.7 Decreased Cardiac Output in Patients With Preserved Left Ventricular Systolic Function
Patients with heart failure associated with preserved left ventricular ejection fraction may experience decreased cardiac output with use of LANOXIN. Such disorders include restrictive cardiomyopathy, constrictive pericarditis, amyloid heart disease, and acute cor pulmonale. Patients with idiopathic hypertrophic subaortic stenosis may have worsening of the outflow obstruction due to the inotropic effects of digoxin. Patients with amyloid heart disease may be more susceptible to digoxin toxicity at therapeutic levels because of an increased binding of digoxin to extracellular amyloid fibrils.
LANOXIN should generally be avoided in these patients, although it has been used for ventricular rate control in the subgroup of patients with atrial fibrillation.
5.8 Reduced Efficacy In Patients With Hypocalcemia
Hypocalcemia can nullify the effects of digoxin in humans; thus, digoxin may be ineffective until serum calcium is restored to normal. These interactions are related to the fact that digoxin affects contractility and excitability of the heart in a manner similar to that of calcium.
5.9 Altered Response in Thyroid Disorders and Hypermetabolic States
Hypothyroidism may reduce the requirements for digoxin.
Heart failure and/or atrial arrhythmias resulting from hypermetabolic or hyperdynamic states (e.g., hyperthyroidism, hypoxia, or arteriovenous shunt) are best treated by addressing the underlying condition. Atrial arrhythmias associated with hypermetabolic states are particularly resistant to digoxin treatment. Patients with beri beri heart disease may fail to respond adequately to digoxin if the underlying thiamine deficiency is not treated concomitantly.
-
6 ADVERSE REACTIONS
The following adverse reactions are included in more detail in the Warnings and Precautions section of the label:
- Cardiac arrhythmias [see Warnings and Precautions (5.1, 5.2)]
- Digoxin Toxicity [see Warnings and Precautions (5.3)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in clinical practice.
In general, the adverse reactions of LANOXIN are dose-dependent and occur at doses higher than those needed to achieve a therapeutic effect. Hence, adverse reactions are less common when LANOXIN is used within the recommended dose range, is maintained within the therapeutic serum concentration range, and when there is careful attention to concurrent medications and conditions.
In the DIG trial (a trial investigating the effect of digoxin on mortality and morbidity in patients with heart failure), the incidence of hospitalization for suspected digoxin toxicity was 2% in patients taking LANOXIN compared to 0.9% in patients taking placebo [see Clinical Studies (14.1)].
The overall incidence of adverse reactions with digoxin has been reported as 5-20%, with 15-20% of adverse events considered serious. Cardiac toxicity accounts for about one-half, gastrointestinal disturbances for about one-fourth, and CNS and other toxicity for about one-fourth of these adverse events.
Gastrointestinal: In addition to nausea and vomiting, the use of digoxin has been associated with abdominal pain, intestinal ischemia, and hemorrhagic necrosis of the intestines.
CNS: Digoxin can cause headache, weakness, dizziness, apathy, confusion, and mental disturbances (such as anxiety, depression, delirium, and hallucination).
Other: Gynecomastia has been occasionally observed following the prolonged use of digoxin. Thrombocytopenia and maculopapular rash and other skin reactions have been rarely observed.
-
7 DRUG INTERACTIONS
Digoxin has a narrow therapeutic index, increased monitoring of serum digoxin concentrations and for potential signs and symptoms of clinical toxicity is necessary when initiating, adjusting, or discontinuing drugs that may interact with digoxin. Prescribers should consult the prescribing information of any drug which is co-prescribed with digoxin for potential drug interaction information.
7.1 P-Glycoprotein (PGP) Inducers/Inhibitors
Digoxin is a substrate of P-glycoprotein, at the level of intestinal absorption, renal tubular section and biliary-intestinal secretion. Therefore, drugs that induce/inhibit P-glycoprotein have the potential to alter digoxin pharmacokinetics.
7.2 Pharmacokinetic Drug Interactions
NA – Not available/reported
7.3 Potentially Significant Pharmacodynamic Drug Interactions
Because of considerable variability of pharmacodynamic interactions, the dosage of digoxin should be individualized when patients receive these medications concurrently.
7.4 Drug/Laboratory Test Interactions
Endogenous substances of unknown composition (digoxin-like immunoreactive substances, [DLIS]) can interfere with standard radioimmunoassays for digoxin. The interference most often causes results to be falsely positive or falsely elevated, but sometimes it causes results to be falsely reduced. Some assays are more subject to these failings than others. Several LC/MS/MS methods are available that may provide less susceptibility to DLIS interference. DLIS are present in up to half of all neonates and in varying percentages of pregnant women, patients with hypertrophic cardiomyopathy, patients with renal or hepatic dysfunction, and other patients who are volume-expanded for any reason. The measured levels of DLIS (as digoxin equivalents) are usually low (0.2-0.4 ng/mL), but sometimes they reach levels that would be considered therapeutic or even toxic.
In some assays, spironolactone, canrenone, and potassium canrenoate may be falsely detected as digoxin, at levels up to 0.5 ng/mL. Some traditional Chinese and Ayurvedic medicine substances like Chan Su, Siberian Ginseng, Asian Ginseng, Ashwagandha or Dashen can cause similar interference.
Spironolactone and DLIS are much more extensively protein-bound than digoxin. As a result, assays of free digoxin levels in protein-free ultrafiltrate (which tend to be about 25% less than total levels, consistent with the usual extent of protein binding) are less affected by spironolactone or DLIS. It should be noted that ultrafiltration does not solve all interference problems with alternative medicines. The use of an LC/MS/MS method may be the better option according to the good results it provides, especially in terms of specificity and limit of quantization.
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
Experience with digoxin in pregnant women over several decades, based on published retrospective clinical studies and case reports, has not led to the identification of a drug associated risk of major birth defects, miscarriage or adverse maternal and fetal outcomes. Untreated underlying maternal conditions, such as heart failure and atrial fibrillation, during pregnancy pose a risk to mother and fetus (see clinical consideration). Animal reproduction studies have not been conducted with digoxin.The estimated background risk of major birth defects and miscarriage for the indicated population(s) are unknown. All pregnancies have a background risk of birth defect, loss, or other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2%-4% and 15%-20%, respectively.
Clinical ConsiderationsDisease-associated maternal and/or embryo/fetal risk
Pregnant women with heart failure are at increased risk of preterm birth. Clinical classification of heart disease may worsen with pregnancy and lead to maternal or fetal death.Pregnant women with atrial fibrillation are at increased risk of delivering a low birth weight infant. Atrial fibrillation may worsen with pregnancy and can lead to maternal or fetal death.
Fetal/neonatal adverse reactions
Digoxin has been shown to cross the placenta and is found in amniotic fluid. Monitor neonates for signs and symptoms of digoxin toxicity, including vomitting, cardiac arrhythmias [see Warning and Precautions (5.3)].Dose adjustments during pregnancy and the postpartum period
LANOXIN requirements may increase during pregnancy and decrease in the postpartum period. Monitor serum digoxin levels during pregnancy and postpartum period [see Dosage and Administration (2.5)].Labor or delivery
Risk of arrhythmias may increase duing labor and delivery. Monitor patients continously during labor and delivery [see Warnings and Precautions (5.1and 5.2)].8.2 Lactation
Risk Summary The digoxin dose received through breastfeeding is upto 4% of the neonatal maintenance dosage, which is unlikely to be clinically relevant. There are no data on the effects of digoxin on the breastfed infant or effects on milk production.
Data Based on data from two lactation studies in a total of 13 breastfed infants, the digoxin concentrations in breast milk were between 0.4 — 1.0 ng/ml following 0.25 mg once daily dose of digoxin in the lactating mother. Thus, the amount of digoxin ingested daily by the infants is estimated to be between 0.03 to 0.16 μg/kg/day. This translates to relative infant dose of digoxin between 1 to 7% of maternal weight-adjusted dose and about 0.2 to 4% of the neonatal maintenance dose.
8.4 Pediatric Use
The safety and effectiveness of LANOXIN in the control of ventricular rate in children with atrial fibrillation have not been established.
The safety and effectiveness of LANOXIN in the treatment of heart failure in children have not been established in adequate and well-controlled studies. However, in published literature of children with heart failure of various etiologies (e.g., ventricular septal defects, anthracycline toxicity, patent ductus arteriosus), treatment with digoxin has been associated with improvements in hemodynamic parameters and in clinical signs and symptoms.
Newborn infants display considerable variability in their tolerance to digoxin. Premature and immature infants are particularly sensitive to the effects of digoxin, and the dosage of the drug must not only be reduced but must be individualized according to their degree of maturity.
8.5 Geriatric Use
The majority of clinical experience gained with digoxin has been in the elderly population. This experience has not identified differences in response or adverse effects between the elderly and younger patients. However, this drug is known to be substantially excreted by the kidney, and the risk of toxic reactions to this drug may be greater in patients with impaired renal function. Because elderly patients are more likely to have decreased renal function, care should be taken in dose selection, which should be based on renal function, and it may be useful to monitor renal function [see Dosage and Administration (2.1)].
8.6 Renal Impairment
The clearance of digoxin can be primarily correlated with the renal function as indicated by creatinine clearance. Tables 3 and 5 provide the usual daily maintenance dose requirements for digoxin based on creatinine clearance [see Dosage and Administration (2.3)].
Digoxin is primarily excreted by the kidneys; therefore, patients with impaired renal function require smaller than usual maintenance doses of digoxin [see Dosage and Administration (2.3)]. Because of the prolonged elimination half-life, a longer period of time is required to achieve an initial or new steady-state serum concentration in patients with renal impairment than in patients with normal renal function. If appropriate care is not taken to reduce the dose of digoxin, such patients are at high risk for toxicity, and toxic effects will last longer in such patients than in patients with normal renal function.
8.7 Hepatic Impairment
Plasma digoxin concentrations in patients with acute hepatitis generally fall within the range of profiles in a group of healthy subjects.
8.8 Malabsorption
The absorption of digoxin is reduced in some malabsorption conditions such as chronic diarrhea.
-
10 OVERDOSAGE
10.1 Signs and Symptoms in Adults and Children
The signs and symptoms of toxicity are generally similar to those described in the Adverse Reactions (6.1) but may be more frequent and can be more severe. Signs and symptoms of digoxin toxicity become more frequent with levels above 2 ng/mL. However, in deciding whether a patient’s symptoms are due to digoxin, the clinical state together with serum electrolyte levels and thyroid function are important factors [see Dosage and Administration (2)].
Adults: The most common signs and symptoms of digoxin toxicity are nausea, vomiting, anorexia, and fatigue that occur in 30-70% of patients who are overdosed. Extremely high serum concentrations produce hyperkalemia especially in patients with impaired renal function. Almost every type of cardiac arrhythmia has been associated with digoxin overdose and multiple rhythm disturbances in the same patient are common. Peak cardiac effects occur 3-6 hours following ingestion and may persist for 24 hours or longer. Arrhythmias that are considered more characteristic of digoxin toxicity are new-onset Mobitz type 1 A-V block, accelerated junctional rhythms, non-paroxysmal atrial tachycardia with A-V block, and bi-directional ventricular tachycardia. Cardiac arrest from asystole or ventricular fibrillation is usually fatal.
Digoxin toxicity is related to serum concentration. As digoxin serum levels increase above 1.2 ng/mL, there is a potential for increase in adverse reactions. Furthermore, lower potassium levels increases the risk for adverse reactions. In adults with heart disease, clinical observations suggest that an overdose of digoxin of 10-15 mg results in death of half of patients. A dose above 25 mg ingested by an adult without heart disease appeared to be uniformly fatal if no Digoxin Immune Fab (DIGIBIND®, DIGIFAB®) was administered.
Among the extra-cardiac manifestations, gastrointestinal symptoms (e.g., nausea, vomiting, anorexia) are very common (up to 80% incidence) and precede cardiac manifestations in approximately half of the patients in most literature reports. Neurologic manifestations (e.g., dizziness, various CNS disturbances), fatigue, and malaise are very common. Visual manifestations may also occur with aberration in color vision (predominance of yellow green) the most frequent. Neurological and visual symptoms may persist after other signs of toxicity have resolved. In chronic toxicity, non-specific extra-cardiac symptoms, such as malaise and weakness, may predominate.
Children: In pediatric patients, signs and symptoms of toxicity can occur during or shortly after the dose of digoxin. Frequent non-cardiac effects are similar to those observed in adults although nausea and vomiting are not seen frequently in infants and small pediatric patients. Other reported manifestations of overdose are weight loss in older age groups, failure to thrive in infants, abdominal pain caused by mesenteric artery ischemia, drowsiness, and behavioral disturbances including psychotic episodes. Arrhythmias and combinations of arrhythmias that occur in adult patients can also occur in pediatric patients although sinus tachycardia, supraventricular tachycardia, and rapid atrial fibrillation are seen less frequently in pediatric patients. Pediatric patients are more likely to develop A-V conduction disturbances, or sinus bradycardia. Any arrhythmia in a child treated with digoxin should be considered related to digoxin until otherwise ruled out. In pediatric patients aged 1-3 years without heart disease, clinical observations suggest that an overdose of digoxin of 6-10 mg would result in death of half of the patients. In the same population, a dose above 10 mg resulted in death if no Digoxin Immune Fab were administered.
10.2 Treatment
Chronic Overdose
If there is suspicion of toxicity, discontinue LANOXIN and place the patient on a cardiac monitor. Correct factors such as electrolyte abnormalities, thyroid dysfunction, and concomitant medications [see Dosage and Administration (2.5)]. Correct hypokalemia by administering potassium so that serum potassium is maintained between 4.0 and 5.5 mmol/L. Potassium is usually administered orally, but when correction of the arrhythmia is urgent and serum potassium concentration is low, potassium may be administered by the intravenous route. Monitor electrocardiogram for any evidence of potassium toxicity (e.g., peaking of T waves) and to observe the effect on the arrhythmia. Avoid potassium salts in patients with bradycardia or heart block. Symptomatic arrhythmias may be treated with Digoxin Immune Fab.
Acute Overdose
Patients who have intentionally or accidently ingested massive doses of digoxin should receive activated charcoal orally or by nasogastric tube regardless of the time since ingestion since digoxin recirculates to the intestine by enterohepatic circulation. In addition to cardiac monitoring, temporarily discontinue LANOXIN until the adverse reaction resolves. Correct factors that may be contributing to the adverse reactions [see Warnings and Precautions (5)]. In particular, correct hypokalemia and hypomagnesemia. Digoxin is not effectively removed from the body by dialysis because of its large extravascular volume of distribution. Life threatening arrhythmias (ventricular tachycardia, ventricular fibrillation, high degree A-V block, bradyarrhythma, sinus arrest) or hyperkalemia requires administration of Digoxin Immune Fab. Digoxin Immune Fab has been shown to be 80-90% effective in reversing signs and symptoms of digoxin toxicity. Bradycardia and heart block caused by digoxin are parasympathetically mediated and respond to atropine. A temporary cardiac pacemaker may also be used. Ventricular arrhythmias may respond to lidocaine or phenytoin. When a large amount of digoxin has been ingested, especially in patients with impaired renal function, hyperkalemia may be present due to release of potassium from skeletal muscle. In this case, treatment with Digoxin Immune Fab is indicated; an initial treatment with glucose and insulin may be needed if the hyperkalemia is life-threatening. Once the adverse reaction has resolved, therapy with LANOXIN may be reinstituted following a careful reassessment of dose.
-
11 DESCRIPTION
LANOXIN (digoxin) is one of the cardiac (or digitalis) glycosides, a closely related group of drugs having in common specific effects on the myocardium. These drugs are found in a number of plants. Digoxin is extracted from the leaves of Digitalis lanata. The term “digitalis” is used to designate the whole group of glycosides. The glycosides are composed of 2 portions: a sugar and a cardenolide (hence “glycosides”).
Digoxin is described chemically as (3β,5β,12β)-3-[(O-2,6-dideoxy-β-D-ribo-hexopyranosyl-(1→4)-O-2,6-dideoxy-β-D-ribo-hexopyranosyl-(1→4)-2,6-dideoxy-β-D—ribo-hexopyranosyl)oxy]-12,14-dihydroxy-card-20(22)-enolide. Its molecular formula is C41H64O14, its molecular weight is 780.95, and its structural formula is:
Digoxin exists as odorless white crystals that melt with decomposition above 230°C. The drug is practically insoluble in water and in ether; slightly soluble in diluted (50%) alcohol and in chloroform; and freely soluble in pyridine.
LANOXIN is supplied as 62.5 mcg (unscored), 125 mcg (scored), and 250 mcg (scored) tablets for oral administration. Each tablet contains the labeled amount of digoxin USP and the following inactive ingredients: corn and potato starches, lactose and magnesium stearate. The 125 mcg tablets contain D&C Yellow No. 10 and FD&C Yellow No. 6, and the 62.5 mcg tablets contain FD&C Yellow No. 6.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
All of digoxin’s actions are mediated through its effects on Na-K ATPase. This enzyme, the “sodium pump,” is responsible for maintaining the intracellular milieu throughout the body by moving sodium ions out of and potassium ions into cells. By inhibiting Na-K ATPase, digoxin
- causes increased availability of intracellular calcium in the myocardium and conduction system, with consequent increased inotropy, increased automaticity, and reduced conduction velocity
- indirectly causes parasympathetic stimulation of the autonomic nervous system, with consequent effects on the sino-atrial (SA) and atrioventricular (AV) nodes
- reduces catecholamine reuptake at nerve terminals, rendering blood vessels more sensitive to endogenous or exogenous catecholamines
- increases baroreceptor sensitization, with consequent increased carotid sinus nerve activity and enhanced sympathetic withdrawal for any given increment in mean arterial pressure
- increases (at higher concentrations) sympathetic outflow from the central nervous system (CNS) to both cardiac and peripheral sympathetic nerves
- allows (at higher concentrations) progressive efflux of intracellular potassium, with consequent increase in serum potassium levels.
The cardiologic consequences of these direct and indirect effects are an increase in the force and velocity of myocardial systolic contraction (positive inotropic action), a slowing of the heart rate (negative chronotropic effect), decreased conduction velocity through the AV node, and a decrease in the degree of activation of the sympathetic nervous system and renin-angiotensin system (neurohormonal deactivating effect).
12.2 Pharmacodynamics
The times to onset of pharmacologic effect and to peak effect of preparations of LANOXIN are shown in Table 7.
a Documented for ventricular response rate in atrial fibrillation, inotropic effects and electrocardiographic changes.
b Depending upon rate of infusion.Hemodynamic Effects: Short- and long-term therapy with the drug increases cardiac output and lowers pulmonary artery pressure, pulmonary capillary wedge pressure, and systemic vascular resistance in patients with heart failure. These hemodynamic effects are accompanied by an increase in the left ventricular ejection fraction and a decrease in end-systolic and end-diastolic dimensions.
ECG Changes: The use of therapeutic doses of LANOXIN may cause prolongation of the PR interval and depression of the ST segment on the electrocardiogram. LANOXIN may produce false positive ST-T changes on the electrocardiogram during exercise testing. These electrophysiologic effects are not indicative of toxicity. LANOXIN does not significantly reduce heart rate during exercise.
12.3 Pharmacokinetics
Note: The following data are from studies performed in adults, unless otherwise stated.
Absorption: Following oral administration, peak serum concentrations of digoxin occur at 1 to 3 hours. Absorption of digoxin from LANOXIN Tablets has been demonstrated to be 60-80% complete compared to an identical intravenous dose of digoxin (absolute bioavailability). When LANOXIN Tablets are taken after meals, the rate of absorption is slowed, but the total amount of digoxin absorbed is usually unchanged. When taken with meals high in bran fiber, however, the amount absorbed from an oral dose may be reduced. Comparisons of the systemic availability and equivalent doses for oral preparations of LANOXIN are shown in Dosage and Administration (2.6).
Digoxin is a substrate for P-glycoprotein. As an efflux protein on the apical membrane of enterocytes, P-glycoprotein may limit the absorption of digoxin.
In some patients, orally administered digoxin is converted to inactive reduction products (e.g., dihydrodigoxin) by colonic bacteria in the gut. Data suggest that 1 in 10 patients treated with digoxin tablets, colonic bacteria will degrade 40% or more of the ingested dose. As a result, certain antibiotics may increase the absorption of digoxin in such patients. Although inactivation of these bacteria by antibiotics is rapid, the serum digoxin concentration will rise at a rate consistent with the elimination half-life of digoxin. Serum digoxin concentration relates to the extent of bacterial inactivation, and may be as much as doubled in some cases [see Drug Interactions (7.2)].
Patients with malabsorption syndromes (e.g., short bowel syndrome, celiac sprue, jejunoileal bypass) may have a reduced ability to absorb orally administered digoxin.
Distribution: Following drug administration, a 6-8 hour tissue distribution phase is observed. This is followed by a much more gradual decline in the serum concentration of the drug, which is dependent on the elimination of digoxin from the body. The peak height and slope of the early portion (absorption/distribution phases) of the serum concentration-time curve are dependent upon the route of administration and the absorption characteristics of the formulation. Clinical evidence indicates that the early high serum concentrations do not reflect the concentration of digoxin at its site of action, but that with chronic use, the steady-state post-distribution serum concentrations are in equilibrium with tissue concentrations and correlate with pharmacologic effects. In individual patients, these post-distribution serum concentrations may be useful in evaluating therapeutic and toxic effects [see Dosage and Administration (2.1)].
Digoxin is concentrated in tissues and therefore has a large apparent volume of distribution (approximately 475-500 L). Digoxin crosses both the blood-brain barrier and the placenta. At delivery, the serum digoxin concentration in the newborn is similar to the serum concentration in the mother. Approximately 25% of digoxin in the plasma is bound to protein. Serum digoxin concentrations are not significantly altered by large changes in fat tissue weight, so that its distribution space correlates best with lean (i.e., ideal) body weight, not total body weight.
Metabolism: Only a small percentage (13%) of a dose of digoxin is metabolized in healthy volunteers. The urinary metabolites, which include dihydrodigoxin, digoxigenin bisdigitoxoside, and their glucuronide and sulfate conjugates, are polar in nature and are postulated to be formed via hydrolysis, oxidation, and conjugation. The metabolism of digoxin is not dependent upon the cytochrome P-450 system, and digoxin is not known to induce or inhibit the cytochrome P-450 system.
Excretion: Elimination of digoxin follows first-order kinetics (that is, the quantity of digoxin eliminated at any time is proportional to the total body content). Following intravenous administration to healthy volunteers, 50-70% of a digoxin dose is excreted unchanged in the urine. Renal excretion of digoxin is proportional to creatinine clearance and is largely independent of urine flow. In healthy volunteers with normal renal function, digoxin has a half-life of 1.5-2 days. The half-life in anuric patients is prolonged to 3.5-5 days. Digoxin is not effectively removed from the body by dialysis, exchange transfusion, or during cardiopulmonary bypass because most of the drug is bound to extravascular tissues.
Special Populations: Geriatrics: Because of age-related declines in renal function, elderly patients would be expected to eliminate digoxin more slowly than younger subjects. Elderly patients may also exhibit a lower volume of distribution of digoxin due to age-related loss of lean muscle mass. Thus, the dosage of digoxin should be carefully selected and monitored in elderly patients [see Use in Specific Populations (8.5)].
Gender: In a study of 184 patients, the clearance of digoxin was 12% lower in female than in male patients. This difference is not likely to be clinically important.
Hepatic Impairment: Because only a small percentage (approximately 13%) of a dose of digoxin undergoes metabolism, hepatic impairment would not be expected to significantly alter the pharmacokinetics of digoxin. In a small study, plasma digoxin concentration profiles in patients with acute hepatitis generally fell within the range of profiles in a group of healthy subjects. No dosage adjustments are recommended for patients with hepatic impairment; however, serum digoxin concentrations should be used as appropriate to help guide dosing in these patients.
Renal Impairment: Since the clearance of digoxin correlates with creatinine clearance, patients with renal impairment generally demonstrate prolonged digoxin elimination half-lives and greater exposures to digoxin. Therefore, titrate carefully in these patients based on clinical response, and based on monitoring of serum digoxin concentrations, as appropriate.
Race: The impact of race differences on digoxin pharmacokinetics have not been formally studied. Because digoxin is primarily eliminated as unchanged drug via the kidney and because there are no important differences in creatinine clearance among races, pharmacokinetic differences due to race are not expected.
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Digoxin showed no genotoxic potential in in vitro studies (Ames test and mouse lymphoma). No data are available on the carcinogenic potential of digoxin, nor have studies been conducted to assess its potential to affect fertility.
-
14 CLINICAL STUDIES
14.1 Chronic Heart Failure
Two 12-week, double-blind, placebo-controlled studies enrolled 178 (RADIANCE trial) and 88 (PROVED trial) adult patients with NYHA Class II or III heart failure previously treated with oral digoxin, a diuretic, and an ACE inhibitor (RADIANCE only) and randomized them to placebo or treatment with LANOXIN Tablets. Both trials demonstrated better preservation of exercise capacity in patients randomized to LANOXIN. Continued treatment with LANOXIN reduced the risk of developing worsening heart failure, as evidenced by heart failure-related hospitalizations and emergency care and the need for concomitant heart failure therapy.
DIG Trial of LANOXIN in Patients with Heart Failure
The Digitalis Investigation Group (DIG) main trial was a 37-week, multicenter, randomized, double-blind mortality study comparing digoxin to placebo in 6800 adult patients with heart failure and left ventricular ejection fraction less than or equal to 0.45. At randomization, 67% were NYHA class I or II, 71% had heart failure of ischemic etiology, 44% had been receiving digoxin, and most were receiving a concomitant ACE inhibitor (94%) and diuretics (82%). As in the smaller trials described above, patients who had been receiving open-label digoxin were withdrawn from this treatment before randomization. Randomization to digoxin was again associated with a significant reduction in the incidence of hospitalization, whether scored as number of hospitalizations for heart failure (relative risk 75%), risk of having at least one such hospitalization during the trial (RR 72%), or number of hospitalizations for any cause (RR 94%). On the other hand, randomization to digoxin had no apparent effect on mortality (RR 99%, with confidence limits of 91-107%).
14.2 Chronic Atrial Fibrillation
Digoxin has also been studied as a means of controlling the ventricular response to chronic atrial fibrillation in adults. Digoxin reduced the resting heart rate, but not the heart rate during exercise.
In 3 different randomized, double-blind trials that included a total of 315 adult patients, digoxin was compared to placebo for the conversion of recent-onset atrial fibrillation to sinus rhythm. Conversion was equally likely, and equally rapid, in the digoxin and placebo groups. In a randomized 120-patient trial comparing digoxin, sotalol, and amiodarone, patients randomized to digoxin had the lowest incidence of conversion to sinus rhythm, and the least satisfactory rate control when conversion did not occur.
In at least one study, digoxin was studied as a means of delaying reversion to atrial fibrillation in adult patients with frequent recurrence of this arrhythmia. This was a randomized, double-blind, 43-patient crossover study. Digoxin increased the mean time between symptomatic recurrent episodes by 54%, but had no effect on the frequency of fibrillatory episodes seen during continuous electrocardiographic monitoring.
-
16 HOW SUPPLIED/STORAGE AND HANDLING
LANOXIN Tablets have «LANOXIN» on one side and are supplied as follows:
Store at 25°C (77°F); excursions permitted to 15 to 30°C (59 to 86°F) [See USP Controlled Room Temperature] in a dry place and protect from light. Keep out of reach of children.
Dispense in tight, light-resistant container. -
17 PATIENT COUNSELING INFORMATION
- Advise patients that many drugs can interact with LANOXIN. Instruct patients to inform their doctor and pharmacist if they are taking any over the counter medications, including herbal medication, or are started on a new prescription.
- Advise patients to contact their doctor or a health care professional if they experience nausea, vomiting, persistent diarrhea, confusion, weakness, or visual disturbances (including blurred vision, green-yellow color disturbances, halo effect) as these could be signs that the dose of LANOXIN may be too high.
- Advise parents or caregivers that the symptoms of having too high LANOXIN doses may be difficult to recognize in infants and pediatric patients. Symptoms such as weight loss, failure to thrive in infants, abdominal pain, and behavioral disturbances may be indications of digoxin toxicity.
- Instruct the patient to monitor and record their heart rate and blood pressure daily.
LANOXIN is a registered trademark of GlaxoSmithKline.
Manufactured for:
Advanz Pharma (US) Corp.
Bannockburn, IL 60015©2024. All rights reserved.
-
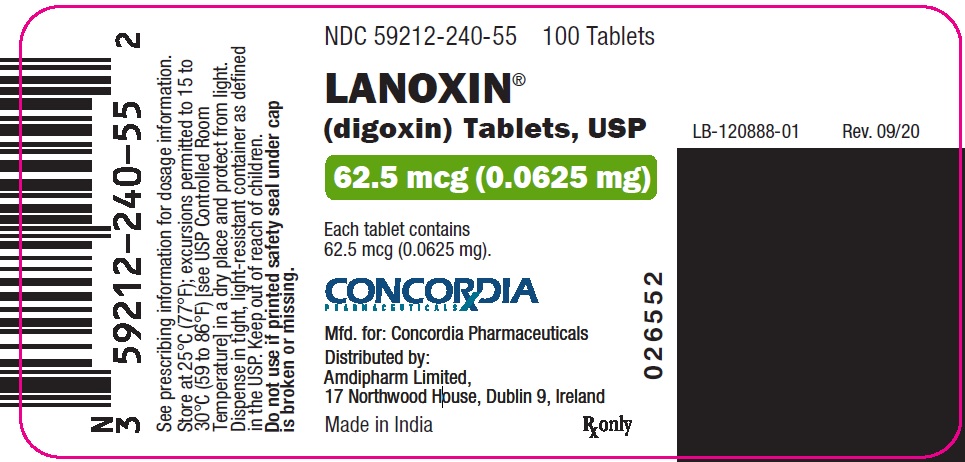
PRINCIPAL DISPLAY PANEL — 62.5 mcg
NDC 59212-240-55 100 Tablets
LANOXIN®
(digoxin) Tablets, USP62.5 mcg
ADVANZ PHARMA
Manufactured for:
Advanz Pharma (US) Corp.
Bannockburn, IL 60015
Made in India RX only -
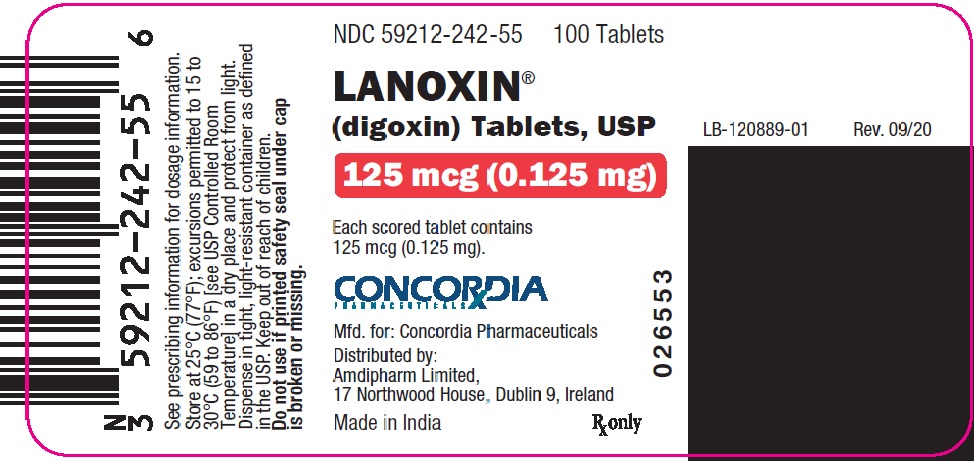
PRINCIPAL DISPLAY PANEL — 125 mcg
NDC 59212-242-55 100 Tablets
LANOXIN®
(digoxin) Tablets, USP125 mcg
ADVANZ PHARMA
Manufactured for:
Advanz Pharma (US) Corp.
Bannockburn, IL 60015
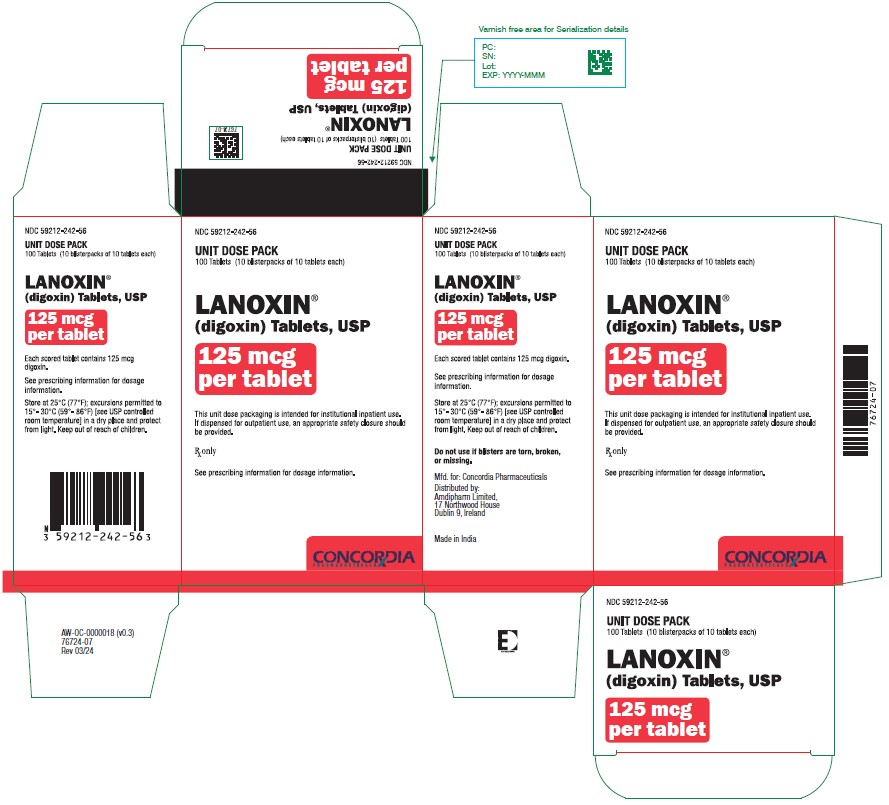
Made in India RX onlyNDC 59212-242-56
UNIT DOSE PACK
100 Tablets (10 blister packs of 10 tablets each)LANOXIN®
(digoxin) Tablets, USP125 mcg per tablet
This unit dose packaging is intended for institutional inpatient use.
If dispensed for outpatient use, an appropriate safety closure should be provided.RX only
ADVANZ PHARMA
See prescribing information for dosage information.
-
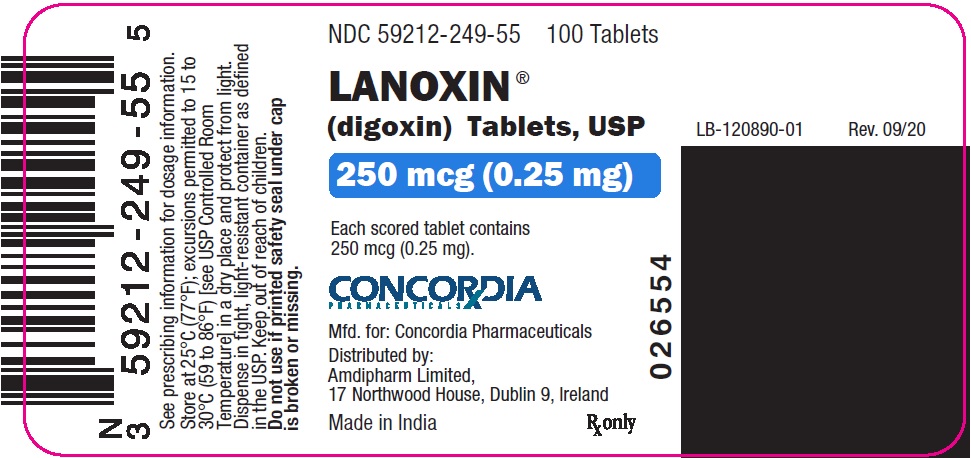
PRINCIPAL DISPLAY PANEL — 250 mcg
NDC 59212-249-55 100 Tablets
LANOXIN®
(digoxin) Tablets, USP250 mcg
ADVANZ PHARMA
Manufactured for:
Advanz Pharma (US) Corp.
Bannockburn, IL 60015
Made in India RX only
adagrasib will increase the level or effect of digoxin by P-glycoprotein (MDR1) efflux transporter. Avoid or Use Alternate Drug. Avoid coadministration of adagrasib, a P-gp inhibitor, with sensitive P-gp substrates unless otherwise recommended in the prescribing information for these substrates.
aluminum hydroxide will increase the level or effect of digoxin by increasing gastric pH. Applies only to oral form of both agents. Avoid or Use Alternate Drug.
amiodarone will increase the level or effect of digoxin by P-glycoprotein (MDR1) efflux transporter. Avoid or Use Alternate Drug. Amiodarone increases PO digoxin serum concentrations by ~70% and IV digoxin by ~17%; measure digoxin levels before initiating amiodarone and reduce PO digoxin dose by 30-50%; decrease IV digoxin dose by 15-30%amiodarone will increase the level or effect of digoxin by basic (cationic) drug competition for renal tubular clearance. Avoid or Use Alternate Drug. Amiodarone increases PO digoxin serum concentrations by ~70% and IV digoxin by ~17%; measure digoxin levels before initiating amiodarone and reduce PO digoxin dose by 30-50%; decrease IV digoxin dose by 15-30%
amphotericin B deoxycholate increases effects of digoxin by pharmacodynamic synergism. Avoid or Use Alternate Drug. Digoxin effects increased if hypokalemia results from Ampho B Tx.
digoxin, atenolol.
Either decreases toxicity of the other by unspecified interaction mechanism. Avoid or Use Alternate Drug. Can increase risk of bradycardia.
azithromycin will increase the level or effect of digoxin by altering intestinal flora. Applies only to oral form of both agents. Avoid or Use Alternate Drug.
digoxin, betaxolol.
Either increases toxicity of the other by unspecified interaction mechanism. Avoid or Use Alternate Drug. Can increase risk of bradycardia.
digoxin, bisoprolol.
Either decreases toxicity of the other by unspecified interaction mechanism. Avoid or Use Alternate Drug. Can increase risk of bradycardia.
bremelanotide will decrease the level or effect of digoxin by Other (see comment). Avoid or Use Alternate Drug. Bremelanotide may slow gastric emptying and potentially reduces the rate and extent of absorption of concomitantly administered oral medications. Avoid use when taking any oral drug that is dependent on threshold concentrations for efficacy. Interactions listed are representative examples and do not include all possible clinical examples.
bretylium increases toxicity of digoxin by sympathetic (adrenergic) effects, including increased blood pressure and heart rate. Avoid or Use Alternate Drug. Avoid simultaneous initiation of therapy with digitalis glycosides and bretylium. Initial release of norepinephrine caused by bretylium may aggravate digitalis toxicity. When a life-threatening cardiac arrhythmia occurs in a digitalized patient, bretylium should be used only if the etiology of the arrhythmia does not appear to be digitalis toxicity and other antiarrhythmic drugs are not effective. Bretylium is contraindicated for digitalis-induced arrhythmias.
calcium carbonate will increase the level or effect of digoxin by increasing gastric pH. Applies only to oral form of both agents. Avoid or Use Alternate Drug.
ceftobiprole medocaril sodium will increase the level or effect of digoxin by Other (see comment). Avoid or Use Alternate Drug. Ceftobiprole (an OATP1B1/1B3 inhibitor) may increase plasma concentrations of OATP1B1 and OATP1B3 substrates.
clarithromycin will increase the level or effect of digoxin by altering intestinal flora. Applies only to oral form of both agents. Avoid or Use Alternate Drug.
colchicine, digoxin.
Either increases toxicity of the other by unspecified interaction mechanism. Avoid or Use Alternate Drug. Increased risk of rhabdomyolysis.
cyclosporine increases levels of digoxin by decreasing renal clearance. Avoid or Use Alternate Drug.
dexlansoprazole will increase the level or effect of digoxin by increasing gastric pH. Applies only to oral form of both agents. Avoid or Use Alternate Drug.
digoxin will increase the level or effect of dofetilide by basic (cationic) drug competition for renal tubular clearance. Avoid or Use Alternate Drug.
digoxin increases levels of eluxadoline by decreasing metabolism. Avoid or Use Alternate Drug. Decrease eluxadoline dose to 75 mg PO BID if coadministered with OATP1B1 inhibitors. .
enasidenib will increase the level or effect of digoxin by Other (see comment). Avoid or Use Alternate Drug. Avoid coadministration of enasidenib with sensitive OATP1B1, OATP1B3, or BCRP substrates, for which minimal concentration changes may lead to serious toxicities. If unavoidable, decrease the substrate(s) dosage in accordance with their Prescribing Information.
erdafitinib will increase the level or effect of digoxin by P-glycoprotein (MDR1) efflux transporter. Avoid or Use Alternate Drug. If coadministration unavoidable, separate administration by at least 6 hr before or after administration of P-gp substrates with narrow therapeutic index.
erythromycin base will increase the level or effect of digoxin by altering intestinal flora. Applies only to oral form of both agents. Avoid or Use Alternate Drug.
erythromycin ethylsuccinate will increase the level or effect of digoxin by altering intestinal flora. Applies only to oral form of both agents. Avoid or Use Alternate Drug.
erythromycin lactobionate will increase the level or effect of digoxin by altering intestinal flora. Applies only to oral form of both agents. Avoid or Use Alternate Drug.
erythromycin stearate will increase the level or effect of digoxin by altering intestinal flora. Applies only to oral form of both agents. Avoid or Use Alternate Drug.
digoxin, esmolol.
Either decreases toxicity of the other by unspecified interaction mechanism. Avoid or Use Alternate Drug. Can increase risk of bradycardia.
esomeprazole will increase the level or effect of digoxin by increasing gastric pH. Applies only to oral form of both agents. Avoid or Use Alternate Drug.
famotidine will increase the level or effect of digoxin by increasing gastric pH. Applies only to oral form of both agents. Avoid or Use Alternate Drug.
flecainide increases effects of digoxin by unknown mechanism. Avoid or Use Alternate Drug.
hydroxychloroquine sulfate increases levels of digoxin by unknown mechanism. Avoid or Use Alternate Drug.
ibuprofen/famotidine will increase the level or effect of digoxin by increasing gastric pH. Applies only to oral form of both agents. Avoid or Use Alternate Drug.
landiolol, digoxin.
Either increases effects of the other by pharmacodynamic synergism. Avoid or Use Alternate Drug. Coadministration of beta blockers with other negative inotropes or chronotropes may augment myocardial contractility depression and increase risk of bradycardia or heart block.
lansoprazole will increase the level or effect of digoxin by increasing gastric pH. Applies only to oral form of both agents. Avoid or Use Alternate Drug.
lasmiditan increases levels of digoxin by P-glycoprotein (MDR1) efflux transporter. Avoid or Use Alternate Drug.
leniolisib will increase the level or effect of digoxin by Other (see comment). Avoid or Use Alternate Drug. Leniolisib, an OATP1B1 and OATP1B3 inhibitor, may increase systemic exposure of these substrates
digoxin, levobunolol.
Either increases toxicity of the other by unspecified interaction mechanism. Avoid or Use Alternate Drug. Can increase risk of bradycardia.
digoxin, lily of the valley.
Either increases toxicity of the other by pharmacodynamic synergism. Contraindicated.
digoxin increases toxicity of metoprolol by unspecified interaction mechanism. Avoid or Use Alternate Drug. Can increase risk of bradycardia.
digoxin, nadolol.
Either increases toxicity of the other by unspecified interaction mechanism. Avoid or Use Alternate Drug. Can increase risk of bradycardia.
digoxin, nebivolol.
Either decreases toxicity of the other by unspecified interaction mechanism. Avoid or Use Alternate Drug. Can increase risk of bradycardia.
nizatidine will increase the level or effect of digoxin by increasing gastric pH. Applies only to oral form of both agents. Avoid or Use Alternate Drug.
omeprazole will increase the level or effect of digoxin by increasing gastric pH. Applies only to oral form of both agents. Avoid or Use Alternate Drug.
ozanimod increases toxicity of digoxin by sympathetic (adrenergic) effects, including increased blood pressure and heart rate. Avoid or Use Alternate Drug. Because the active metabolite of ozanimod inhibits MAO-B in vitro, there is a potential for serious adverse reactions, including hypertensive crisis. Therefore, coadministration of ozanimod with drugs that can increase norepinephrine or serotonin is not recommended. Monitor for hypertension with concomitant use.
pacritinib will increase the level or effect of digoxin by P-glycoprotein (MDR1) efflux transporter. Avoid or Use Alternate Drug.
pantoprazole will increase the level or effect of digoxin by increasing gastric pH. Applies only to oral form of both agents. Avoid or Use Alternate Drug.
ponesimod, digoxin.
Either increases effects of the other by pharmacodynamic synergism. Avoid or Use Alternate Drug. Consult cardiologist if considering treatment. Coadministration of ponesimod with drugs that decrease HR may have additive effects on decreasing HR and should generally not be initiated in these patients.
digoxin will increase the level or effect of procainamide by basic (cationic) drug competition for renal tubular clearance. Avoid or Use Alternate Drug.
propafenone increases levels of digoxin by decreasing renal clearance. Avoid or Use Alternate Drug.
digoxin, propranolol.
Either increases toxicity of the other by unspecified interaction mechanism. Avoid or Use Alternate Drug. Can increase risk of bradycardia.
quinidine will increase the level or effect of digoxin by P-glycoprotein (MDR1) efflux transporter. Avoid or Use Alternate Drug.quinidine will increase the level or effect of digoxin by basic (cationic) drug competition for renal tubular clearance. Avoid or Use Alternate Drug.
rabeprazole will increase the level or effect of digoxin by increasing gastric pH. Applies only to oral form of both agents. Avoid or Use Alternate Drug.
roxithromycin will increase the level or effect of digoxin by altering intestinal flora. Applies only to oral form of both agents. Avoid or Use Alternate Drug.
siponimod, digoxin.
Either increases effects of the other by pharmacodynamic synergism. Avoid or Use Alternate Drug. Because of the potential additive effects on heart rate, siponimod should generally not be initiated in patients taking QT prolonging drugs with known arrhythmogenic properties, heart rate lowering calcium channel blockers, or other drugs that may decrease heart rate. If treatment considered, obtain cardiology consult regarding switching to non-heart-rate lowering drugs or appropriate monitoring for treatment initiation.
sodium bicarbonate will increase the level or effect of digoxin by increasing gastric pH. Applies only to oral form of both agents. Avoid or Use Alternate Drug.
sodium citrate/citric acid will increase the level or effect of digoxin by increasing gastric pH. Applies only to oral form of both agents. Avoid or Use Alternate Drug.
digoxin, sotalol.
Either increases toxicity of the other by unspecified interaction mechanism. Avoid or Use Alternate Drug. Can increase risk of bradycardia.
sotorasib will decrease the level or effect of digoxin by P-glycoprotein (MDR1) efflux transporter. Avoid or Use Alternate Drug. If use is unavoidable, refer to the prescribing information of the P-gp substrate for dosage modifications.
sucralfate will decrease the level or effect of digoxin by inhibition of GI absorption. Applies only to oral form of both agents. Avoid or Use Alternate Drug. Measure serum digoxin concentrations before initiating concomitant drugs; continue monitoring and increase digoxin dose by approximately 20% to 40% as necessary
tepotinib will increase the level or effect of digoxin by P-glycoprotein (MDR1) efflux transporter. Avoid or Use Alternate Drug. If concomitant use unavoidable, reduce the P-gp substrate dosage if recommended in its approved product labeling.
digoxin, timolol.
Either increases toxicity of the other by unspecified interaction mechanism. Avoid or Use Alternate Drug. Can increase risk of bradycardia.
trofinetide will increase the level or effect of digoxin by Other (see comment). Avoid or Use Alternate Drug. Trofinetide (an OATP131 and OATP13B inhibitor) may increase plasma levels of OATP131 or OATP13B substrates. Avoid coadministration with sensitive substrates.
vandetanib increases levels of digoxin by P-glycoprotein (MDR1) efflux transporter. Avoid or Use Alternate Drug.
venetoclax will increase the level or effect of digoxin by P-glycoprotein (MDR1) efflux transporter. Avoid or Use Alternate Drug. In vitro data suggest venetoclax may inhibit P-gp substrates at therapeutic dose levels in the gut. Avoid coadministration of narrow therapeutic index P-gp substrates with venetoclax. If a narrow therapeutic index P-gp substrate must be used, it should be taken at least 6 hr before venetoclax.
verapamil increases levels of digoxin by decreasing renal clearance. Avoid or Use Alternate Drug.
abrocitinib will increase the level or effect of digoxin by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor. Monitor and titrate dose of P-gp substrate appropriately.
acarbose will decrease the level or effect of digoxin by unspecified interaction mechanism. Use Caution/Monitor. Measure serum digoxin concentrations before initiating concomitant drugs; continue monitoring and increase digoxin dose by approximately 20% to 40% as necessary
acebutolol and digoxin both increase serum potassium. Use Caution/Monitor.acebutolol increases effects of digoxin by pharmacodynamic synergism. Use Caution/Monitor. Enhanced bradycardia.
aceclofenac and digoxin both increase serum potassium. Use Caution/Monitor.
acemetacin and digoxin both increase serum potassium. Use Caution/Monitor.
activated charcoal decreases levels of digoxin by inhibition of GI absorption. Applies only to oral form of both agents. Use Caution/Monitor.
digoxin increases and albuterol decreases serum potassium. Effect of interaction is not clear, use caution. Use Caution/Monitor.
alprazolam increases levels of digoxin by unknown mechanism. Use Caution/Monitor.
amikacin will increase the level or effect of digoxin by altering intestinal flora. Applies only to oral form of both agents. Use Caution/Monitor.
amiloride and digoxin both increase serum potassium. Modify Therapy/Monitor Closely.
anticholinergic/sedative combos increases levels of digoxin by unspecified interaction mechanism. Use Caution/Monitor.
digoxin increases and arformoterol decreases serum potassium. Effect of interaction is not clear, use caution. Use Caution/Monitor.
aspirin and digoxin both increase serum potassium. Use Caution/Monitor.
aspirin rectal and digoxin both increase serum potassium. Use Caution/Monitor.
aspirin/citric acid/sodium bicarbonate and digoxin both increase serum potassium. Use Caution/Monitor.
atazanavir increases effects of digoxin by pharmacodynamic synergism. Use Caution/Monitor. Increased risk of AV block.
atenolol and digoxin both increase serum potassium. Use Caution/Monitor.atenolol increases effects of digoxin by pharmacodynamic synergism. Use Caution/Monitor. Enhanced bradycardia.
atorvastatin will increase the level or effect of digoxin by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor.
atropine increases levels of digoxin by unknown mechanism. Use Caution/Monitor.
atropine IV/IM increases levels of digoxin by unknown mechanism. Use Caution/Monitor.
aztreonam will increase the level or effect of digoxin by altering intestinal flora. Applies only to oral form of both agents. Use Caution/Monitor.
benazepril increases levels of digoxin by unspecified interaction mechanism. Use Caution/Monitor.
digoxin increases and bendroflumethiazide decreases serum potassium. Effect of interaction is not clear, use caution. Use Caution/Monitor.bendroflumethiazide increases effects of digoxin by pharmacodynamic synergism. Use Caution/Monitor. Hypokalemia increases digoxin effects.
benzgalantamine, digoxin.
Either increases effects of the other by pharmacodynamic synergism. Modify Therapy/Monitor Closely. Galantamine, an acetylcholinesterase inhibitor, has vagotonic effects on the SA and AV nodes, leading to bradycardia. Consider consulting a cardiolist before initiating other drugs that may cause bradycardia.
berotralstat will increase the level or effect of digoxin by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor. Monitor or titrate P-gp substrate dose if coadministered.
betaxolol and digoxin both increase serum potassium. Use Caution/Monitor.betaxolol increases effects of digoxin by pharmacodynamic synergism. Use Caution/Monitor. Enhanced bradycardia.
bisoprolol and digoxin both increase serum potassium. Use Caution/Monitor.bisoprolol increases effects of digoxin by pharmacodynamic synergism. Use Caution/Monitor. Enhanced bradycardia.
bosutinib increases levels of digoxin by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor.
brimonidine increases effects of digoxin by pharmacodynamic synergism. Use Caution/Monitor.
digoxin increases and bumetanide decreases serum potassium. Effect of interaction is not clear, use caution. Use Caution/Monitor.bumetanide increases effects of digoxin by pharmacodynamic synergism. Use Caution/Monitor. Hypokalemia increases digoxin effects.
bupropion will decrease the level or effect of digoxin by Other (see comment). Use Caution/Monitor. Monitor for decreased digoxin concentrations; bupropion may induce OATP4C1 transporter, which is involved in digoxin renal elimination
calcifediol, digoxin. Other (see comment). Modify Therapy/Monitor Closely.
Comment: Calcifediol may cause hypercalcemia which would increase the risk of digitalis toxicity. Monitor both serum calcium levels and for signs and symptoms of digitalis toxicity.
calcium acetate increases effects of digoxin by pharmacodynamic synergism. Use Caution/Monitor.
calcium carbonate increases effects of digoxin by pharmacodynamic synergism. Use Caution/Monitor.
calcium chloride increases effects of digoxin by pharmacodynamic synergism. Use Caution/Monitor.
calcium citrate increases effects of digoxin by pharmacodynamic synergism. Use Caution/Monitor.
calcium gluconate increases effects of digoxin by pharmacodynamic synergism. Use Caution/Monitor.
canagliflozin increases levels of digoxin by unspecified interaction mechanism. Modify Therapy/Monitor Closely. Digoxin AUC and peak serum concentration increased when coadministered with canagliflozin.
candesartan and digoxin both increase serum potassium. Use Caution/Monitor.
cannabidiol will increase the level or effect of digoxin by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor. Therapeutic drug monitoring and dose reduction of P-gp substrates should be considered when given orally and concurrently with cannabidiol
captopril increases levels of digoxin by unspecified interaction mechanism. Use Caution/Monitor.
digoxin increases and carbenoxolone decreases serum potassium. Effect of interaction is not clear, use caution. Use Caution/Monitor.
carmustine decreases levels of digoxin by inhibition of GI absorption. Applies only to oral form of both agents. Use Caution/Monitor. It is prudent to closely monitor patients for loss of clinical efficacy of digoxin while receiving antineoplastic therapy.
carvedilol and digoxin both increase serum potassium. Use Caution/Monitor.carvedilol increases levels of digoxin by enhancing GI absorption. Applies only to oral form of both agents. Use Caution/Monitor.carvedilol increases levels of digoxin by decreasing renal clearance. Use Caution/Monitor.carvedilol increases effects of digoxin by pharmacodynamic synergism. Use Caution/Monitor. Enhanced bradycardia.
cefadroxil will increase the level or effect of digoxin by altering intestinal flora. Applies only to oral form of both agents. Use Caution/Monitor.
cefamandole will increase the level or effect of digoxin by altering intestinal flora. Applies only to oral form of both agents. Use Caution/Monitor.
cefpirome will increase the level or effect of digoxin by altering intestinal flora. Applies only to oral form of both agents. Use Caution/Monitor.
cefpodoxime will increase the level or effect of digoxin by altering intestinal flora. Applies only to oral form of both agents. Use Caution/Monitor.
celecoxib and digoxin both increase serum potassium. Use Caution/Monitor.
celiprolol and digoxin both increase serum potassium. Use Caution/Monitor.celiprolol increases effects of digoxin by pharmacodynamic synergism. Use Caution/Monitor. Enhanced bradycardia.
cephalexin will increase the level or effect of digoxin by altering intestinal flora. Applies only to oral form of both agents. Use Caution/Monitor.
chlorhexidine oral will increase the level or effect of digoxin by altering intestinal flora. Applies only to oral form of both agents. Use Caution/Monitor.
digoxin increases and chlorothiazide decreases serum potassium. Effect of interaction is not clear, use caution. Use Caution/Monitor.chlorothiazide increases effects of digoxin by pharmacodynamic synergism. Use Caution/Monitor. Hypokalemia increases digoxin effects.
digoxin increases and chlorthalidone decreases serum potassium. Effect of interaction is not clear, use caution. Use Caution/Monitor.chlorthalidone increases effects of digoxin by pharmacodynamic synergism. Use Caution/Monitor. Hypokalemia increases digoxin effects.
cholestyramine decreases levels of digoxin by inhibition of GI absorption. Applies only to oral form of both agents. Use Caution/Monitor.
choline magnesium trisalicylate and digoxin both increase serum potassium. Use Caution/Monitor.
clarithromycin will increase the level or effect of digoxin by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor.
clindamycin will increase the level or effect of digoxin by altering intestinal flora. Applies only to oral form of both agents. Use Caution/Monitor.
clotrimazole will decrease the level or effect of digoxin by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor.
cobicistat will increase the level or effect of digoxin by P-glycoprotein (MDR1) efflux transporter. Modify Therapy/Monitor Closely. Measure serum digoxin concentrations before initiating concomitant drugs. Titrate the digoxin dose by ~30-50% or by modifying the dosing frequency and continue monitoring.
colestipol decreases levels of digoxin by inhibition of GI absorption. Applies only to oral form of both agents. Use Caution/Monitor.
conivaptan increases levels of digoxin by decreasing metabolism. Use Caution/Monitor.
crizotinib increases levels of digoxin by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Use Caution/Monitor. Coadministration of crizotinib with CYP3A substrates with narrow therapeutic indices should be avoided.crizotinib increases levels of digoxin by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor.
digoxin increases and cyclopenthiazide decreases serum potassium. Effect of interaction is not clear, use caution. Use Caution/Monitor.cyclopenthiazide increases effects of digoxin by pharmacodynamic synergism. Use Caution/Monitor. Hypokalemia increases digoxin effects.
cyclophosphamide decreases levels of digoxin by inhibition of GI absorption. Applies only to oral form of both agents. Use Caution/Monitor.
cyclosporine will increase the level or effect of digoxin by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor.
cytarabine decreases levels of digoxin by inhibition of GI absorption. Applies only to oral form of both agents. Use Caution/Monitor. Cytarabine may decrease digoxin absorption even several days after stopping chemotherapy. Digoxin capsules and digitoxin do not appear to be affected. .
danicopan will increase the level or effect of digoxin by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor. Danicopan increases plasma concentrations of P-gp substrates; consider dose reduction of P-gp substrates where minimal concentration changes may lead to serious adverse reactions.
dapsone will increase the level or effect of digoxin by altering intestinal flora. Applies only to oral form of both agents. Use Caution/Monitor.
darifenacin increases levels of digoxin by unspecified interaction mechanism. Use Caution/Monitor.
demeclocycline will increase the level or effect of digoxin by altering intestinal flora. Applies only to oral form of both agents. Use Caution/Monitor.
dexlansoprazole increases toxicity of digoxin by Other (see comment). Use Caution/Monitor.
Comment: Prolonged use of PPIs may cause hypomagnesemia and increase risk for digoxin toxicity.
dichlorphenamide and digoxin both decrease serum potassium. Use Caution/Monitor.
diclofenac and digoxin both increase serum potassium. Use Caution/Monitor.
diflunisal and digoxin both increase serum potassium. Use Caution/Monitor.
diphenoxylate hcl will increase the level or effect of digoxin by unspecified interaction mechanism. Use Caution/Monitor. Measure serum digoxin concentrations before initiating concomitant drugs; continue monitoring and reduce digoxin dose as necessary
digoxin increases and dobutamine decreases serum potassium. Effect of interaction is not clear, use caution. Use Caution/Monitor.
dopamine increases toxicity of digoxin by pharmacodynamic synergism. Use Caution/Monitor. Can increase risk of cardiac arrhythmias.
digoxin increases and dopexamine decreases serum potassium. Effect of interaction is not clear, use caution. Use Caution/Monitor.
doxorubicin decreases levels of digoxin by inhibition of GI absorption. Applies only to oral form of both agents. Use Caution/Monitor.
doxorubicin liposomal decreases levels of digoxin by inhibition of GI absorption. Applies only to oral form of both agents. Use Caution/Monitor.
doxycycline will increase the level or effect of digoxin by altering intestinal flora. Applies only to oral form of both agents. Use Caution/Monitor.
dronedarone will increase the level or effect of digoxin by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor. If coadministered, consider reducing digoxin dose. Closely monitor serum digoxin levels and observe for digoxin toxicity.
drospirenone and digoxin both increase serum potassium. Modify Therapy/Monitor Closely.
dulaglutide, digoxin. Other (see comment). Use Caution/Monitor.
Comment: Dulaglutide slows gastric emptying and may impact absorption of concomitantly administered oral medications; be particularly cautious when coadministered with drugs that have a narrow therapeutic index.
elacestrant will increase the level or effect of digoxin by P-glycoprotein (MDR1) efflux transporter. Modify Therapy/Monitor Closely. Reduce dose of P-gp substrates per their Prescribing Information when minimal concentration changes may lead to serious or life-threatening adverse reactions.
elagolix will increase the level or effect of digoxin by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor.
eliglustat increases levels of digoxin by P-glycoprotein (MDR1) efflux transporter. Modify Therapy/Monitor Closely. Measure digoxin levels before initiating eliglustat and reduce digoxin dose by 30%; continue to monitor digoxin levels and adjust dose accordingly.
elvitegravir/cobicistat/emtricitabine/tenofovir DF increases levels of digoxin by P-glycoprotein (MDR1) efflux transporter. Modify Therapy/Monitor Closely. Digoxin is a substrate for P-gp transport; cobicistat inhibits P-gp transport; initiate digoxin at low dose and carefully titrate.
enalapril increases levels of digoxin by unspecified interaction mechanism. Use Caution/Monitor.
encorafenib will increase the level or effect of digoxin by Other (see comment). Modify Therapy/Monitor Closely. Encorafenib (a OATP1B1 and OATP1B3 inhibitor) may increase the concentration and toxicities of OATP1B1 and OATP1B3 substrates. Closely monitor for signs and symptoms of increased exposure and consider adjusting the dose of these substrates.
digoxin increases and ephedrine decreases serum potassium. Effect of interaction is not clear, use caution. Use Caution/Monitor.
digoxin increases and epinephrine decreases serum potassium. Effect of interaction is not clear, use caution. Use Caution/Monitor.
epinephrine intranasal, digoxin.
Either increases effects of the other by pharmacodynamic synergism. Use Caution/Monitor. Observe for cardiac arrhythmias if epinephrine is coadministered with cardiac glycosides, diuretics, or antiarrhythmic drugs. .
digoxin increases and epinephrine racemic decreases serum potassium. Effect of interaction is not clear, use caution. Use Caution/Monitor.
epoprostenol will increase the level or effect of digoxin by unspecified interaction mechanism. Use Caution/Monitor. Measure serum digoxin concentrations before initiating concomitant drugs; continue monitoring and reduce digoxin dose as necessary
eprosartan and digoxin both increase serum potassium. Use Caution/Monitor.
eribulin will decrease the level or effect of digoxin by Other (see comment). Use Caution/Monitor. Antineoplastic agents may decrease absorption of digoxin; monitor patients for therapeutic efficacy.
ertapenem will increase the level or effect of digoxin by altering intestinal flora. Applies only to oral form of both agents. Use Caution/Monitor.
erythromycin base will increase the level or effect of digoxin by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor.
erythromycin ethylsuccinate will increase the level or effect of digoxin by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor.
erythromycin lactobionate will increase the level or effect of digoxin by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor.
erythromycin stearate will increase the level or effect of digoxin by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor.
esmolol and digoxin both increase serum potassium. Use Caution/Monitor.esmolol increases effects of digoxin by pharmacodynamic synergism. Use Caution/Monitor. Enhanced bradycardia.
esomeprazole increases toxicity of digoxin by Other (see comment). Use Caution/Monitor.
Comment: Prolonged use of PPIs may cause hypomagnesemia and increase risk for digoxin toxicity.
digoxin increases and ethacrynic acid decreases serum potassium. Effect of interaction is not clear, use caution. Use Caution/Monitor.ethacrynic acid increases effects of digoxin by pharmacodynamic synergism. Use Caution/Monitor. Hypokalemia increases digoxin effects.
etodolac and digoxin both increase serum potassium. Use Caution/Monitor.
etravirine increases levels of digoxin by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor. Potential for increased toxicity. .
ezogabine increases levels of digoxin by decreasing renal clearance. Use Caution/Monitor. Active metabolite, NAMR, may inhibit the renal tubular secretion. Monitor digoxin levels.
famciclovir increases levels of digoxin by unspecified interaction mechanism. Use Caution/Monitor. Coadministration increases digoxin Cmax by ~19%.
felodipine will increase the level or effect of digoxin by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor.
fenoprofen and digoxin both increase serum potassium. Use Caution/Monitor.
ferric maltol, digoxin.
Either increases levels of the other by unspecified interaction mechanism. Modify Therapy/Monitor Closely. Coadministration of ferric maltol with certain oral medications may decrease the bioavailability of either ferric maltol and some oral drugs. For oral drugs where reductions in bioavailability may cause clinically significant effects on its safety or efficacy, separate administration of ferric maltol from these drugs. Duration of separation may depend on the absorption of the medication concomitantly administered (eg, time to peak concentration, whether the drug is an immediate or extended release product).
fleroxacin will increase the level or effect of digoxin by altering intestinal flora. Applies only to oral form of both agents. Use Caution/Monitor.
flibanserin increases levels of digoxin by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor. Increase monitoring of concentrations of drugs transported by P-gp that have a narrow therapeutic index if coadministered with flibanserin.
flurbiprofen and digoxin both increase serum potassium. Use Caution/Monitor.
digoxin increases and formoterol decreases serum potassium. Effect of interaction is not clear, use caution. Use Caution/Monitor.
fosfomycin will increase the level or effect of digoxin by altering intestinal flora. Applies only to oral form of both agents. Use Caution/Monitor.
fosinopril increases levels of digoxin by unspecified interaction mechanism. Use Caution/Monitor.
fosphenytoin will decrease the level or effect of digoxin by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor.
fostamatinib will increase the level or effect of digoxin by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor. Concomitant use of fostamatinib may increase concentrations of P-gp substrates. Monitor for toxicities of the P-gp substrate drug that may require dosage reduction when given concurrently with fostamatinib.
fostemsavir will increase the level or effect of digoxin by Other (see comment). Modify Therapy/Monitor Closely. Fostemsavir inhibits OATP1B1/3 transporter. If possible, avoid coadministration or modify dose of OATP1B1/3 substrates coadministered with fostemsavir.
digoxin increases and furosemide decreases serum potassium. Effect of interaction is not clear, use caution. Use Caution/Monitor.furosemide increases effects of digoxin by pharmacodynamic synergism. Use Caution/Monitor. Hypokalemia increases digoxin effects.
galantamine, digoxin.
Either increases effects of the other by pharmacodynamic synergism. Modify Therapy/Monitor Closely. Galantamine, an acetylcholinesterase inhibitor, has vagotonic effects on the SA and AV nodes, leading to bradycardia. Consider consulting a cardiolist before initiating other drugs that may cause bradycardia.
gemifloxacin will increase the level or effect of digoxin by altering intestinal flora. Applies only to oral form of both agents. Use Caution/Monitor.
gentamicin will increase the level or effect of digoxin by altering intestinal flora. Applies only to oral form of both agents. Use Caution/Monitor.digoxin increases and gentamicin decreases serum potassium. Effect of interaction is not clear, use caution. Use Caution/Monitor.
gepotidacin increases levels of digoxin by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor. Consider monitoring digoxin serum concentrations, as appropriate, if coadministered. .
glecaprevir/pibrentasvir will increase the level or effect of digoxin by P-glycoprotein (MDR1) efflux transporter. Modify Therapy/Monitor Closely. Measure serum digoxin concentrations before initiating glecaprevir/pibrentasvir. To reduce digoxin concentrations, decrease the dose by ~50% or by modifying the dosing frequency and continue monitoring.
glycopyrrolate increases levels of digoxin by unknown mechanism. Use Caution/Monitor.
glycopyrrolate inhaled increases levels of digoxin by unknown mechanism. Use Caution/Monitor.
hawthorn increases effects of digoxin by pharmacodynamic synergism. Use Caution/Monitor.
digoxin will increase the level or effect of hydrochlorothiazide by basic (cationic) drug competition for renal tubular clearance. Use Caution/Monitor.digoxin increases and hydrochlorothiazide decreases serum potassium. Effect of interaction is not clear, use caution. Use Caution/Monitor.hydrochlorothiazide increases effects of digoxin by pharmacodynamic synergism. Use Caution/Monitor. Hypokalemia increases digoxin effects.
ibuprofen and digoxin both increase serum potassium. Use Caution/Monitor.
ibuprofen IV and digoxin both increase serum potassium. Use Caution/Monitor.
imidapril increases levels of digoxin by unspecified interaction mechanism. Use Caution/Monitor.
digoxin increases and indapamide decreases serum potassium. Effect of interaction is not clear, use caution. Use Caution/Monitor.indapamide increases effects of digoxin by pharmacodynamic synergism. Use Caution/Monitor. Hypokalemia increases digoxin effects.
indomethacin and digoxin both increase serum potassium. Use Caution/Monitor.
irbesartan and digoxin both increase serum potassium. Use Caution/Monitor.
isavuconazonium sulfate will increase the level or effect of digoxin by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor.
digoxin increases and isoproterenol decreases serum potassium. Effect of interaction is not clear, use caution. Use Caution/Monitor.
istradefylline will increase the level or effect of digoxin by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor. Istradefylline 40 mg/day increased peak levels and AUC of P-gp substrates in clinical trials. Consider dose reduction of sensitive P-gp substrates.
itraconazole will increase the level or effect of digoxin by P-glycoprotein (MDR1) efflux transporter. Modify Therapy/Monitor Closely. Measure digoxin levels before initiating concomitant drugs. Monitor and consider reducing the digoxin dose by ~30-50% or modifying the dosing frequency.
ivabradine, digoxin.
Either increases effects of the other by pharmacodynamic synergism. Modify Therapy/Monitor Closely. Most patients receiving ivabradine will also be treated with a beta-blocker. The risk of bradycardia increases with coadministration of drugs that slow heart rate (eg, digoxin, amiodarone, beta-blockers). Monitor heart rate in patients taking ivabradine with other negative chronotropes.
ivacaftor increases levels of digoxin by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor. Ivacaftor and its M1 metabolite has the potential to inhibit P-gp; may significantly increase systemic exposure to sensitive P-gp substrates with a narrow therapeutic index.
ketoconazole will increase the level or effect of digoxin by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor.
ketoprofen and digoxin both increase serum potassium. Use Caution/Monitor.
ketorolac and digoxin both increase serum potassium. Use Caution/Monitor.
ketorolac intranasal and digoxin both increase serum potassium. Use Caution/Monitor.
labetalol and digoxin both increase serum potassium. Use Caution/Monitor.labetalol increases effects of digoxin by pharmacodynamic synergism. Use Caution/Monitor. Enhanced bradycardia.
lansoprazole increases toxicity of digoxin by Other (see comment). Use Caution/Monitor.
Comment: Prolonged use of PPIs may cause hypomagnesemia and increase risk for digoxin toxicity.
lapatinib will increase the level or effect of digoxin by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor.
ledipasvir/sofosbuvir will increase the level or effect of digoxin by P-glycoprotein (MDR1) efflux transporter. Modify Therapy/Monitor Closely.
lenacapavir will increase the level or effect of digoxin by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Use Caution/Monitor. Use with caution and monitor digoxin therapeutic concentration.
levacetylleucine increases levels of digoxin by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor. Levacetylleucine inhibits P-gp; however, clinical significance of this finding has not been fully characterized. .
digoxin increases and levalbuterol decreases serum potassium. Effect of interaction is not clear, use caution. Use Caution/Monitor.
levofloxacin will increase the level or effect of digoxin by altering intestinal flora. Applies only to oral form of both agents. Use Caution/Monitor.
levoketoconazole will increase the level or effect of digoxin by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor.
levothyroxine decreases effects of digoxin by unknown mechanism. Use Caution/Monitor.
linezolid will increase the level or effect of digoxin by altering intestinal flora. Applies only to oral form of both agents. Use Caution/Monitor.
liothyronine decreases effects of digoxin by unknown mechanism. Use Caution/Monitor.
lisinopril increases levels of digoxin by unspecified interaction mechanism. Use Caution/Monitor.
lomitapide increases levels of digoxin by P-glycoprotein (MDR1) efflux transporter. Modify Therapy/Monitor Closely. Consider reducing dose when used concomitantly with lomitapide.
lonafarnib will increase the level or effect of digoxin by P-glycoprotein (MDR1) efflux transporter. Modify Therapy/Monitor Closely. Lonafarnib is a weak P-gp inhibitor. Monitor for adverse reactions if coadministered with P-gp substrates where minimal concentration changes may lead to serious or life-threatening toxicities. Reduce P-gp substrate dose if needed.
loratadine will increase the level or effect of digoxin by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor.
lornoxicam and digoxin both increase serum potassium. Use Caution/Monitor.
losartan and digoxin both increase serum potassium. Use Caution/Monitor.
lumacaftor/ivacaftor, digoxin. P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor. Lumacaftor has the potential to both inhibit and induce P-gp. Additionally, a clinical study with ivacaftor monotherapy showed that ivacaftor is a weak inhibitor of P-gp.
mavorixafor will increase the level or effect of digoxin by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor. Caution if mavorixafor (a P-gp inhibitor) is coadministered with a sensitive P-gp substrate where minimal substrate concentration changes may lead to serious adverse effects.
meclofenamate and digoxin both increase serum potassium. Use Caution/Monitor.
mefenamic acid and digoxin both increase serum potassium. Use Caution/Monitor.
meloxicam and digoxin both increase serum potassium. Use Caution/Monitor.
digoxin will increase the level or effect of memantine by basic (cationic) drug competition for renal tubular clearance. Use Caution/Monitor.
meropenem will increase the level or effect of digoxin by altering intestinal flora. Applies only to oral form of both agents. Use Caution/Monitor.
meropenem/vaborbactam will increase the level or effect of digoxin by altering intestinal flora. Applies only to oral form of both agents. Use Caution/Monitor.
digoxin increases and metaproterenol decreases serum potassium. Effect of interaction is not clear, use caution. Use Caution/Monitor.
digoxin, metformin.
Either increases levels of the other by basic (cationic) drug competition for renal tubular clearance. Use Caution/Monitor. Measure serum digoxin concentrations before initiating metformin. Monitor patients who take both metformin and digoxin for possible digoxin toxicity and lactic acidosis. Reduce the digoxin and/or metformin dose as necessary.
methotrexate decreases levels of digoxin by inhibition of GI absorption. Applies only to oral form of both agents. Use Caution/Monitor. Serum levels of digoxin may be reduced and actions may be decreased. Monitor patient for signs of reduction in pharmacologic effect of digoxin and increase digoxin dose if necessary. Serum level monitoring may facilitate tailoring dosage.
digoxin will increase the level or effect of methyclothiazide by basic (cationic) drug competition for renal tubular clearance. Use Caution/Monitor.digoxin increases and methyclothiazide decreases serum potassium. Effect of interaction is not clear, use caution. Use Caution/Monitor. .methyclothiazide increases effects of digoxin by pharmacodynamic synergism. Use Caution/Monitor. Hypokalemia increases digoxin effects.
metipranolol ophthalmic increases effects of digoxin by pharmacodynamic synergism. Use Caution/Monitor.
metoclopramide decreases levels of digoxin by inhibition of GI absorption. Applies only to oral form of both agents. Use Caution/Monitor.
metoclopramide intranasal will increase the level or effect of digoxin by Other (see comment). Use Caution/Monitor. Metoclopramide may decrease the absorption of digoxin. Monitor therapeutic drug concentrations and increase the digoxin dose as needed.
digoxin increases and metolazone decreases serum potassium. Effect of interaction is not clear, use caution. Use Caution/Monitor.metolazone increases effects of digoxin by pharmacodynamic synergism. Use Caution/Monitor. Hypokalemia increases digoxin effects.
metoprolol and digoxin both increase serum potassium. Use Caution/Monitor.metoprolol increases effects of digoxin by pharmacodynamic synergism. Use Caution/Monitor. Enhanced bradycardia.
metronidazole will increase the level or effect of digoxin by altering intestinal flora. Applies only to oral form of both agents. Use Caution/Monitor.
digoxin will increase the level or effect of midodrine by basic (cationic) drug competition for renal tubular clearance. Use Caution/Monitor.
mineral oil decreases levels of digoxin by inhibition of GI absorption. Applies only to oral form of both agents. Use Caution/Monitor.
minocycline will increase the level or effect of digoxin by altering intestinal flora. Applies only to oral form of both agents. Use Caution/Monitor.
mirabegron will increase the level or effect of digoxin by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor.
moexipril increases levels of digoxin by unspecified interaction mechanism. Use Caution/Monitor.
moxifloxacin will increase the level or effect of digoxin by altering intestinal flora. Applies only to oral form of both agents. Use Caution/Monitor.
nabumetone and digoxin both increase serum potassium. Use Caution/Monitor.
nadolol and digoxin both increase serum potassium. Use Caution/Monitor.nadolol increases effects of digoxin by pharmacodynamic synergism. Use Caution/Monitor. Enhanced bradycardia.
nafcillin will increase the level or effect of digoxin by altering intestinal flora. Applies only to oral form of both agents. Use Caution/Monitor.
naproxen and digoxin both increase serum potassium. Use Caution/Monitor.
nebivolol and digoxin both increase serum potassium. Use Caution/Monitor.nebivolol increases effects of digoxin by pharmacodynamic synergism. Use Caution/Monitor. Enhanced bradycardia.
nefazodone will increase the level or effect of digoxin by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor.
neomycin PO will increase the level or effect of digoxin by altering intestinal flora. Applies only to oral form of both agents. Use Caution/Monitor.neomycin PO decreases levels of digoxin by inhibition of GI absorption. Applies only to oral form of both agents. Use Caution/Monitor.
neratinib increases levels of digoxin by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor. Neratinib inhibits P-gp transport. Caution if coadministered with a P-gp substrate with a narrow therapeutic index.
nicardipine will increase the level or effect of digoxin by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor.
nifedipine will increase the level or effect of digoxin by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor. Nifedipine may decrease digoxin clearance, increasing plasma concentrations and the risk of toxicity. Adjust the digoxin dose as needed.
nilotinib will increase the level or effect of digoxin by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor.
nirmatrelvir/ritonavir will increase the level or effect of digoxin by P-glycoprotein (MDR1) efflux transporter. Modify Therapy/Monitor Closely. Measure serum digoxin concentrations before initiating nirmatrelvir/ritonavir. Decrease digoxin dose by ~30-50% or by modifying dosing frequency and continue monitoring during coadministration.
nitrofurantoin will increase the level or effect of digoxin by altering intestinal flora. Applies only to oral form of both agents. Use Caution/Monitor.
digoxin increases and norepinephrine decreases serum potassium. Effect of interaction is not clear, use caution. Use Caution/Monitor.
ofloxacin will increase the level or effect of digoxin by altering intestinal flora. Applies only to oral form of both agents. Use Caution/Monitor.digoxin will increase the level or effect of ofloxacin by basic (cationic) drug competition for renal tubular clearance. Use Caution/Monitor.
olmesartan and digoxin both increase serum potassium. Use Caution/Monitor.
omeprazole increases toxicity of digoxin by Other (see comment). Use Caution/Monitor.
Comment: Prolonged use of PPIs may cause hypomagnesemia and increase risk for digoxin toxicity.
oxaprozin and digoxin both increase serum potassium. Use Caution/Monitor.
oxymetazoline topical decreases effects of digoxin by pharmacodynamic synergism. Use Caution/Monitor. Digoxin reduces catecholamine reuptake at nerve terminals, rendering blood vessels more sensitive to endogenous or exogenous catecholamines.
oxytetracycline will increase the level or effect of digoxin by altering intestinal flora. Applies only to oral form of both agents. Use Caution/Monitor.
palopegteriparatide, digoxin. Other (see comment). Modify Therapy/Monitor Closely.
Comment: Hypercalcemia may predispose patients to digitalis toxicity. Parathyroid hormone may transiently increase serum calcium. Consider potential onset of signs and symptoms of digitalis toxicity if coadministered. .
pantoprazole increases toxicity of digoxin by Other (see comment). Use Caution/Monitor.
Comment: Prolonged use of PPIs may cause hypomagnesemia and increase risk for digoxin toxicity.
parecoxib and digoxin both increase serum potassium. Use Caution/Monitor.
paricalcitol increases toxicity of digoxin by pharmacodynamic synergism. Use Caution/Monitor.
paromomycin will increase the level or effect of digoxin by altering intestinal flora. Applies only to oral form of both agents. Use Caution/Monitor.
perindopril increases levels of digoxin by unspecified interaction mechanism. Use Caution/Monitor.
phenobarbital will decrease the level or effect of digoxin by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor.
phenytoin will decrease the level or effect of digoxin by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor.
pindolol and digoxin both increase serum potassium. Use Caution/Monitor.pindolol increases effects of digoxin by pharmacodynamic synergism. Use Caution/Monitor. Enhanced bradycardia.
digoxin increases and pirbuterol decreases serum potassium. Effect of interaction is not clear, use caution. Use Caution/Monitor.
piroxicam and digoxin both increase serum potassium. Use Caution/Monitor.
pirtobrutinib will increase the level or effect of digoxin by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor. Pirtobrutinib (a P-gp inhibitor) may increase plasma concentrations of sensitive P-gp substrates, which may increase the risk of adverse reactions related to these substrates.
ponatinib increases levels of digoxin by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor.
posaconazole increases levels of digoxin by decreasing metabolism. Use Caution/Monitor.
potassium acid phosphate and digoxin both increase serum potassium. Modify Therapy/Monitor Closely.
potassium chloride and digoxin both increase serum potassium. Modify Therapy/Monitor Closely.
digoxin will increase the level or effect of pramipexole by basic (cationic) drug competition for renal tubular clearance. Use Caution/Monitor.
pretomanid will increase the level or effect of digoxin by Other (see comment). Use Caution/Monitor. Increase monitoring for drug-related adverse effects if pretomanid is coadministered with sensitive OATP1B3 or P-gp substrates.
procarbazine decreases levels of digoxin by inhibition of GI absorption. Applies only to oral form of both agents. Use Caution/Monitor.
propantheline will increase the level or effect of digoxin by unspecified interaction mechanism. Modify Therapy/Monitor Closely. Measure serum digoxin concentrations before initiating concomitant drugs; reduce digoxin dose by approximately 15% to 30% or by modifying dosing frequency and continue monitoring
propranolol and digoxin both increase serum potassium. Use Caution/Monitor.propranolol increases effects of digoxin by pharmacodynamic synergism. Use Caution/Monitor. Enhanced bradycardia.
quercetin will decrease the level or effect of digoxin by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor.
quinapril increases levels of digoxin by unspecified interaction mechanism. Use Caution/Monitor.
digoxin will increase the level or effect of quinine by basic (cationic) drug competition for renal tubular clearance. Use Caution/Monitor.
rabeprazole increases toxicity of digoxin by Other (see comment). Use Caution/Monitor.
Comment: Prolonged use of PPIs may cause hypomagnesemia and increase risk for digoxin toxicity.
ramipril increases levels of digoxin by unspecified interaction mechanism. Use Caution/Monitor.
ranolazine will increase the level or effect of digoxin by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor.ranolazine increases levels of digoxin by decreasing metabolism. Use Caution/Monitor. Ranolazine inhibits P glycoprotein.
regorafenib will decrease the level or effect of digoxin by inhibition of GI absorption. Applies only to oral form of both agents. Modify Therapy/Monitor Closely. Chemotherapy may decrease absorption of digoxin; monitor levels and adjust digoxin dose accordingly
rifabutin decreases levels of digoxin by increasing metabolism. Use Caution/Monitor.
rifampin will decrease the level or effect of digoxin by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor. Reduced digoxin serum concentrations, possibly with a suboptimal therapeutic response, may be seen. rifampin decreases levels of digoxin by increasing metabolism. Use Caution/Monitor.
rifapentine decreases levels of digoxin by increasing metabolism. Use Caution/Monitor.
ritonavir will increase the level or effect of digoxin by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor. Plasma concentrations and pharmacologic effects of digoxin may be increased by ritonavir. Monitor for increased effects of digoxin.ritonavir increases levels of digoxin by decreasing renal clearance. Use Caution/Monitor.ritonavir increases levels of digoxin by decreasing hepatic clearance. Use Caution/Monitor.
rolapitant will increase the level or effect of digoxin by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor. Oral rolapitant (P-gp inhibitor) may increase plasma concentrations of P-gp substrates and may result in potential adverse reactions. Monitor digoxin concentrations with concomitant rolapitant use and adjust dosage if necessary.
sacubitril/valsartan and digoxin both increase serum potassium. Use Caution/Monitor.
salicylates (non-asa) and digoxin both increase serum potassium. Use Caution/Monitor.
digoxin increases and salmeterol decreases serum potassium. Effect of interaction is not clear, use caution. Use Caution/Monitor.
salsalate and digoxin both increase serum potassium. Use Caution/Monitor.
sarecycline will increase the level or effect of digoxin by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor. Monitor for toxicities of P-gp substrates that may require dosage reduction when coadministered with P-gp inhibitors.
senna increases toxicity of digoxin by Other (see comment). Use Caution/Monitor.
Comment: Increased risk of cardiac toxicity due to K+ depletion.
sevelamer decreases levels of digoxin by increasing elimination. Use Caution/Monitor.
simvastatin will increase the level or effect of digoxin by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor.
sirolimus will increase the level or effect of digoxin by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor.
sodium picosulfate/magnesium oxide/anhydrous citric acid decreases levels of digoxin by cation binding in GI tract. Use Caution/Monitor. Take at least 2 hours before and not less than 6 hours after administration of sodium picosulfate, magnesium oxide and anhydrous citric acid to avoid magnesium chelation .
sodium sulfate/?magnesium sulfate/potassium chloride decreases levels of digoxin by inhibition of GI absorption. Applies only to oral form of both agents. Modify Therapy/Monitor Closely. Administer digoxin at least 2 hr before and no less than 6 hr after each dose to avoid chelation with magnesium. .
sodium sulfate/potassium sulfate/magnesium sulfate decreases levels of digoxin by inhibition of GI absorption. Applies only to oral form of both agents. Modify Therapy/Monitor Closely. Administer digoxin at least 2 hr before and no less than 6 hr after each dose to avoid chelation with magnesium. .
sofosbuvir/velpatasvir will increase the level or effect of digoxin by P-glycoprotein (MDR1) efflux transporter. Modify Therapy/Monitor Closely. Velpatasvir inhibits P-gp. Monitor digoxin levels if coadministered. Refer to digoxin prescribing information for monitoring and dose modification recommendations for digoxin concentration increases of <50%.
sotagliflozin will increase the level or effect of digoxin by unspecified interaction mechanism. Modify Therapy/Monitor Closely. Increased exposure of digoxin when coadministered with sotagliflozin 400 mg
sotalol and digoxin both increase serum potassium. Use Caution/Monitor.sotalol increases effects of digoxin by pharmacodynamic synergism. Use Caution/Monitor. Enhanced bradycardia.
spironolactone and digoxin both increase serum potassium. Modify Therapy/Monitor Closely.spironolactone, digoxin. Mechanism: decreasing renal clearance. Use Caution/Monitor. False digoxin assay results may be obtained.spironolactone increases levels of digoxin by Other (see comment). Use Caution/Monitor.
Comment: Spironolactone may cause false elevation of digoxin assay.
St John’s Wort will decrease the level or effect of digoxin by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor.St John’s Wort decreases levels of digoxin by increasing metabolism. Use Caution/Monitor.
stiripentol will increase the level or effect of digoxin by P-glycoprotein (MDR1) efflux transporter. Modify Therapy/Monitor Closely. Consider reducing the dose of P-glycoprotein (P-gp) substrates, if adverse reactions are experienced when administered concomitantly with stiripentol.
streptomycin will increase the level or effect of digoxin by altering intestinal flora. Applies only to oral form of both agents. Use Caution/Monitor.
digoxin and succinylcholine both increase serum potassium. Use Caution/Monitor.succinylcholine, digoxin. Mechanism: unknown. Use Caution/Monitor. Increased risk of cardiac arrhythmias.
sulfadiazine will increase the level or effect of digoxin by altering intestinal flora. Applies only to oral form of both agents. Use Caution/Monitor.
sulfamethoxazole will increase the level or effect of digoxin by altering intestinal flora. Applies only to oral form of both agents. Use Caution/Monitor.sulfamethoxazole will increase the level or effect of digoxin by basic (cationic) drug competition for renal tubular clearance. Use Caution/Monitor.
sulfasalazine and digoxin both increase serum potassium. Use Caution/Monitor.sulfasalazine decreases levels of digoxin by inhibition of GI absorption. Applies only to oral form of both agents. Use Caution/Monitor. Sulfasalazine >2 g/day.
sulfisoxazole will increase the level or effect of digoxin by altering intestinal flora. Applies only to oral form of both agents. Use Caution/Monitor.
sulindac and digoxin both increase serum potassium. Use Caution/Monitor.
suvorexant will increase the level or effect of digoxin by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor. Suvorexant may cause a slight increase in digoxin levels
tacrolimus will increase the level or effect of digoxin by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor.
teduglutide increases levels of digoxin by Other (see comment). Use Caution/Monitor.
Comment: Teduglutide may increase absorption of concomitant PO medications; caution with with drugs requiring titration or those with a narrow therapeutic index; dose adjustment may be necessary.
teicoplanin will increase the level or effect of digoxin by altering intestinal flora. Applies only to oral form of both agents. Use Caution/Monitor.
telmisartan and digoxin both increase serum potassium. Use Caution/Monitor.telmisartan increases levels of digoxin by unknown mechanism. Use Caution/Monitor.
temocillin will increase the level or effect of digoxin by altering intestinal flora. Applies only to oral form of both agents. Use Caution/Monitor.
tenofovir DF increases levels of digoxin by decreasing renal clearance. Use Caution/Monitor. Potential for increased toxicity. .
digoxin increases and terbutaline decreases serum potassium. Effect of interaction is not clear, use caution. Use Caution/Monitor.
teriparatide increases toxicity of digoxin by Other (see comment). Use Caution/Monitor.
Comment: Transient hypercalcemia may predispose to digoxin toxicity (rare case reports).
tetracycline will increase the level or effect of digoxin by altering intestinal flora. Applies only to oral form of both agents. Use Caution/Monitor.
thyroid desiccated decreases effects of digoxin by unknown mechanism. Use Caution/Monitor.
ticagrelor increases levels of digoxin by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor. Ticagrelor inhibits P-glycoprotein transporter. Monitor digoxin levels with initiation of or any change in ticagrelor therapy.
tigecycline will increase the level or effect of digoxin by altering intestinal flora. Applies only to oral form of both agents. Use Caution/Monitor.
timolol and digoxin both increase serum potassium. Use Caution/Monitor.timolol increases effects of digoxin by pharmacodynamic synergism. Use Caution/Monitor. Enhanced bradycardia.
tipranavir increases levels of digoxin by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor. Potential for increased toxicity. .
tirzepatide decreases levels of digoxin by Other (see comment). Use Caution/Monitor.
Comment: GLP1 agonists delay gastrc emptying and may impact the absorption of concomitantly administered oral medications. Monitor patients on oral medications dependent on threshold concentrations for efficacy and those with a narrow therapeutic index. .
tobramycin will increase the level or effect of digoxin by altering intestinal flora. Applies only to oral form of both agents. Use Caution/Monitor.
tolfenamic acid and digoxin both increase serum potassium. Use Caution/Monitor.
tolmetin and digoxin both increase serum potassium. Use Caution/Monitor.
tolvaptan will increase the level or effect of digoxin by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor.digoxin and tolvaptan both increase serum potassium. Use Caution/Monitor.
digoxin increases and torsemide decreases serum potassium. Effect of interaction is not clear, use caution. Use Caution/Monitor.torsemide increases effects of digoxin by pharmacodynamic synergism. Use Caution/Monitor. Hypokalemia increases digoxin effects.
trandolapril increases levels of digoxin by unspecified interaction mechanism. Use Caution/Monitor.
trazodone will decrease the level or effect of digoxin by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor.trazodone increases levels of digoxin by unspecified interaction mechanism. Use Caution/Monitor.
digoxin will increase the level or effect of triamterene by basic (cationic) drug competition for renal tubular clearance. Use Caution/Monitor.triamterene and digoxin both increase serum potassium. Modify Therapy/Monitor Closely.
digoxin decreases effects of trimagnesium citrate anhydrous by increasing renal clearance. Use Caution/Monitor.
trimethoprim will increase the level or effect of digoxin by altering intestinal flora. Applies only to oral form of both agents. Use Caution/Monitor.digoxin will increase the level or effect of trimethoprim by basic (cationic) drug competition for renal tubular clearance. Use Caution/Monitor.
digoxin, trospium chloride.
Either increases levels of the other by decreasing renal clearance. Use Caution/Monitor.
tucatinib will increase the level or effect of digoxin by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor. Consider reducing the dosage of P-gp substrates, where minimal concentration changes may lead to serious or life-threatening toxicities.
ulipristal increases levels of digoxin by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor.
ustekinumab, digoxin. Other (see comment). Use Caution/Monitor.
Comment: Formation of CYP450 enzymes can be altered by increased levels of certain cytokines during chronic inflammation; thus, normalizing the formation of CYP450 enzymes. Upon initiation or discontinuation of ustekinumab in patients who are receiving concomitant CYP450 substrates, particularly those with a narrow therapeutic index, consider monitoring for therapeutic effect.
valsartan will increase the level or effect of digoxin by decreasing renal clearance. Use Caution/Monitor. Monitor digoxin levels closely when coadministered with drugs that may decrease glomerular filtration or tubular secretion.
vancomycin will increase the level or effect of digoxin by altering intestinal flora. Applies only to oral form of both agents. Use Caution/Monitor.
vanzacaftor/tezacaftor/deutivacaftor increases levels of digoxin by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor. Vanzacaftor and deutivacaftor are P-gp inhibitors (in vitro). .
vemurafenib increases levels of digoxin by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor.
verapamil will increase the level or effect of digoxin by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor. Toxicity characterized by gastrointestinal and neuropsychiatric symptoms, and cardiac arrhythmias may result.digoxin will increase the level or effect of verapamil by basic (cationic) drug competition for renal tubular clearance. Use Caution/Monitor.
vibegron increases levels of digoxin by unknown mechanism. Modify Therapy/Monitor Closely. In interaction studies, concomitant administration of vibegron increased digoxin Cmax and AUC by 21% and 11%, respectively. Monitor serum digoxin levels before initiating and during therapy with vibegron. Titrate digoxin dose to obtain desired clinical effect. Continue monitoring digoxin concentrations upon discontinuation of vibegron and adjust digoxin dose as needed.
vincristine decreases levels of digoxin by inhibition of GI absorption. Applies only to oral form of both agents. Use Caution/Monitor.
vincristine liposomal decreases levels of digoxin by inhibition of GI absorption. Applies only to oral form of both agents. Use Caution/Monitor.
vitamin D increases toxicity of digoxin by Other (see comment). Use Caution/Monitor.
Comment: Vitamin D may cause hypercalcemia which may affect the actions of digoxin and/or lead to cardiac arrhythmias.
ЛАНОКСИН
Страна-производитель
Великобритания
Фарм-Группа
Кардиотонические средства-сердечные гликозиды
Производители
Глаксо Вэллком(Великобритания)
Международное название
Дигоксин
Синонимы
Дигоксин, Дигоксин Никомед, Дигоксин ТФТ, Дигоксин-Тева, Дилакор, Диланацин, Ланикор
Лекарственные формы
таблетки 0.25мг
Состав
Активное вещество — дигоксин.
Показания к применению
Застойная недостаточность кровообращения (без гемодинамически значимой обструкции выходного тракта сердца), мерцательная тахиаритмия, суправентрикулярная пароксизмальная тахикардия, трепетание предсердий.
Противопоказания
Гликозидная интоксикация.
Побочное действие
Тошнота, рвота, анорексия, брадикардия, желудочковая экстрасистолия, AV блокада, головная боль, головокружение. Возможно нарушение цветового зрения, снижение остроты зрения, скотомы, макро- и микроопсия, при длительном применении — гинекомастия.
Взаимодействие
Адреномиметики увеличивают вероятность развития аритмии, антиаритмические и антихолинэстеразные препараты — брадикардии, глюкокортикоиды, салуретики и др. средства, способствующие потере калия, препараты кальция — гликозидной интоксикации. Аминазин уменьшает кардиотонический эффект, слабительные, антациды, средства, содержащие алюминий, висмут, магний, — всасывание. Рифампицин и сульфасалазин ускоряют метаболизм.
Передозировка
Симптомы: Аритмия, AV блокада, рвота, тошнота.Лечение: препараты калия, унитиол, этилендиаминтетраацетат.
Особые указания
С осторожностью комбинируют с диуретиками, симпатомиметиками. Следует избегать совместного назначения с амфотерицином В и препаратами кальция.
Литература
1. Энциклопедия лекарств, 2003г2. Энциклопедия лекарств, 2002г. 3. Энциклопедия лекарств, 1999г.